SANG MIN PARK
NOVEMBER 8 2021
I. INTRODUCTION
In this essay, Sang Min Park discusses the impact of COVID-19 and the international sanctions regime on the DPRK healthcare system, trends in global health aid for the DPRK and the role of the ROK, and a future inter-Korean Biomedical Cluster Cooperation model in a post-pandemic era, with implications for cooperative threat reduction (CTR+).
Sang Min Park is chief of Department of Family Medicine, Seoul National University College of Medicine. He leads the health system data science lab at the Department of Biomedical Sciences and is the vice-director of the Institute for Health and Unification Studies of SNU.
Acknowledgements: This paper was presented at the Cooperative Solutions for North Korean Denuclearization Workshops, September 2021, organized by the Asia-Pacific Leadership Network for Nuclear Non-proliferation and Disarmament (APLN). The workshops were sponsored by the ROK Ministry of Unification and the MacArthur Foundation, and supported by the Nuclear Threat Initiative as part of an APLN project on reviewing the potential for an effective Cooperative Threat Reduction plus (CTR+) proposal for the DPRK. It is published by APLN here. The slides presentation is here and a video of the presentation may be viewed here
This study is based on a research report prepared at the request of the Asia-Pacific Leadership Network (APLN), but this is the author’s independent view. Funding for this article was provided partially by the Institute for Peace and Unification Studies (IPUS) at Seoul National University under the project “Laying the Groundwork for Unification” and under the project of “2020 North Korea’s Social Change Survey”. This study was also partially supported by the WFUNA (World Federation of United Nations Associations) Peace Fellows Programme.
The views expressed in this report do not necessarily reflect the official policy or position of the Nautilus Institute. Readers should note that Nautilus seeks a diversity of views and opinions on significant topics in order to identify common ground.
This report is published under a 4.0 International Creative Commons License the terms of which are found here.
Banner image: Child with jaundice at the Provincial Pediatric Hospital in Hamhung City, UNICEF photo, here
II. NAPSNET SPECIAL REPORT BY SANG MIN PARK
THE IMPACT OF COVID-19 ON THE DPRK’S HEALTH SYSTEM AND FUTURE INTER-KOREAN BIOMEDICAL CLUSTER COOPERATION IN THE POST-PANDEMIC ERA
NOVEMBER 8 2021
Introduction
The Democratic People’s Republic of Korea (DPRK) is yet to confirm any official cases of COVID-19. Since the start of the pandemic in January 2020, the DPRK has taken extensive measures to control COVID-19, including imposing strict border controls, a 30-day quarantine for those with COVID-like symptoms, lockdowns of entire counties and cities, and a ban on travel between provinces. Several researchers have summarized the status of COVID-19 in the DPRK, its response to the pandemic, and the pandemic’s impact on the economy and regional security of the DPRK.[1],[2],[3]
This paper will attempt to examine the impact of the COVID-19 pandemic on the DPRK health system as well as its future implications in three major ways: 1) a brief update of the DPRK’s response to COVID-19 epidemic in 2021 and its impacts on the DPRK health system; 2) trends in global health aid to the DPRK during the international sanctions regime and the role of the Republic of Korea (ROK) in the COVID-19 pandemic era; and 3) how to build a sustainable and synergistic horizontal inter-Korean cooperation model in the post-pandemic era.
Update on the DPRK’s COVID-19 Response and its Impact on the DPRK Health System
1) Brief Update on the DPRK’s COVID-19 Response in 2021
The UN-backed global vaccine sharing programme, COVID-19 Vaccines Global Access (COVAX), had planned to deliver 1.7 million doses of the AstraZeneca vaccine to the DPRK by May 2021, but the DPRK has rejected the vaccine due to concerns about potential side effects. Although the DPRK has explored possibilities of alternative drugs, such as the Pfizer and Moderna vaccines, the network of ultra-cold refrigerators for mRNA vaccines might not be operable due to chronic electricity shortages in the DPRK. Therefore, the DPRK may be forced to choose vaccines that can be stored at higher temperatures, such as the AstraZeneca vaccine, the Johnson & Johnson vaccine, or those made in China or Russia.
In addition, vaccine prices are also important for the sake of sustainability. Before the COVID-19 pandemic, developing countries paid a median price of $0.80 per dose for all non-COVID vaccines; mRNA-based COVID-19 vaccines such as Pfizer and Moderna are now sold for up to 50 times this price.[4] In addition, both Pfizer and Moderna have raised the prices of their COVID-19 vaccines in Europe in August 2021. Recently, the Institute for National Security Strategy of the ROK remarked that the DPRK seemed to be reluctant towards Chinese vaccines, but that it had more positive assessments of Russian vaccines. On August 19, 2021, COVAX announced that it had allocated around 3 million doses of the Chinese Sinovac to the DPRK during the latest round of vaccine allocation, but it is uncertain whether Pyongyang will respond to the offer.
In a recent article on the DPRK’s vaccination capabilities based on ideal conditions, researchers suggested that the DPRK could provide its entire population with a single COVID-19 vaccine shot in less than 10 days.[5] The DPRK has shown a high level of vaccination coverage,[6] and was known to have a well-organized national immunization program and a technical assistance plan with the collaboration with United Nations Children’s Fund (UNICEF), World Health Organization (WHO), and Global Alliance for Vaccines and Immunization (GAVI). Like previous socialist countries, the DPRK maintains a household doctor system, where one primary care medical staff is put in charge of 100-130 households in the community.6 WHO also reported that the DPRK had one of the highest staff to population ratios (3.68 physicians per 1,000 in 2018) in the region, compared to 1.98 and 2.41 per 1,000 in China and the ROK, respectively.[7] Under the monolithic centralized administration of the DPRK, this household doctor system might work relatively well to support a vaccination program or maintain quarantine and isolation to prevent the spread of communicable disease.
2) The Impact of the DPRK COVID-19 Response on DPRK’s Health System
Although the DPRK had shown remarkable improvement on several health outcomes such as high level of vaccination coverage, international sanctions brought about due to the DPRK nuclear program have had a catastrophic effect on the economy and the healthcare system; the DPRK’s gross domestic product (GDP) has halved and its healthcare system is chronically underfunded.[8],[9] The DPRK is one of the countries that has benefited the least from global health aid, in spite of its heavy burden of disease.8,[10],[11],[12] The central bank of the ROK reported that the DPRK’s GDP shrank by 4.5% in 2020 – the worst contraction in 23 years – and trade hit a 30-year low after the COVID-19 lockdown.[13]
Several previous studies have documented that many post-socialist countries experienced a lack of healthcare financing, which weakened the public health system and deepened the marketization of healthcare practices.[14],[15] It is likely that the DPRK shares these similarities. A previous study performed by the authors used a mixed-methods approach to analyze the state of the unofficial healthcare market in the DPRK, and found that under-the-table payments and unauthorized private practice among physicians is common.[16],[17] These results are supported by two quantitative surveys on healthcare delivery, dual (private/public) practice, and the unofficial healthcare market in the DPRK, which were carried out in 2011 and 2019 among North Korean defectors who have settled in the ROK.[18]
Officially, healthcare and medicines are provided for free in the DPRK. During the Cold War era, healthcare workers were at the forefront of ideological battles, and DPRK law stated that physicians should take care of patients with “utmost sincerity” in accordance with the “Jung-Sung (Whole Heart) Movement.”16,[19] However, without adequate government support for healthcare providers, the social custom of providing gifts to healthcare workers gradually turned into an unofficial mandatory fee for service. Some healthcare workers even explicitly request bribes from patients.16,17 In addition, the DPRK authorities have tacitly allowed private free markets where people could sell and buy food or other goods since 2000, because the government was unable to manage the distribution of regular food rations.[20] In our in-depth interviews, we found that the diversion of essential medicines from global health aid was very common in the DPRK, and many healthcare providers have been unofficially selling medicine on the private free market.16,17 Although it is illegal to sell medicines in the DPRK, chronic under-funding in health sectors, lack of financial support for healthcare providers, and loosening governmental control over them has led to the emergence of an unofficial healthcare market that has transformed the nature of the healthcare delivery system.
In our quantitative surveys, the percentage of respondents who reported that they had purchased medicines at a private free market was 69% in 2011, and 91% in 2019.18 As for the reason for buying drugs in the informal healthcare market, more than half reported lack of appropriate medicines in hospitals or clinics in 2019, and 19% reported that doctors had told their patients to buy pills in the market. DPRK patients even believed that pills obtained at a hospital might be less effective than those obtained in the market.18
The DPRK is a fragile state with complicated relationships to development partners and the international community as a whole.[21] Under the UN sanctions regime, development aid for health assistance to the DPRK has been limited.10 The unpredictability of health aid could increase the fluctuation of medicine prices due to unforeseeable gaps in supply and demand. In addition, absence of official regulations for the price of medicine could accelerate socioeconomic disparity and unequal access to healthcare in the DPRK. Deepening marketization of healthcare practices without a supplementary social safety system also exacerbates the inequality of healthcare access across different socioeconomic groups, and causes the patient-doctor relationship to become impersonalized.[22] The socioeconomic disparity leads to changes in the patient’s behavior such as self-management of symptoms or delayed access to necessary medical care. Without additional efforts to strengthen the healthcare system in the DPRK, inadequate and unpredictable provision of essential medicines could accelerate the post-socialist transition of its healthcare system.17,[23]
Several previous studies have documented that many post-socialist countries have experienced a lack of healthcare financing, leading to weakening public health system and deepening the marketization of healthcare practices.22,[24] In developing countries with limited health financing, many researchers have demonstrated that healthcare workers who are employed full-time by the government usually take on additional jobs, including private for-profit services.[25],[26] As dual practice of healthcare providers is known to have negative impacts on the health system,[27] it is important to understand the current situation of dual practices in the DPRK.
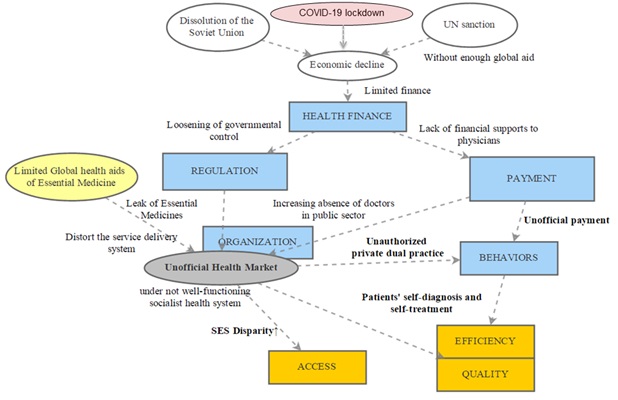
Although we have been unable to collect detailed data on the state of the DPRK’s healthcare system during the COVID-19 pandemic, we assume that the prolonged COVID-19 lockdown measures might worsen the abovementioned trends. Deepening marketization of healthcare practices without a supplementary social safety system seems to exacerbate the inequality of healthcare access between different socioeconomic groups in the DPRK, especially during the COVID pandemic crisis (Figure 1).
Figure 1. A causal loop diagram to illustrate the pathways of the impact of the international sanctions regime and the COVID-19 epidemic on the health system of the DPRK
The expansion of the unofficial medical market, a common phenomenon seen throughout many post-socialist states, is also being observed in the DPRK. This makes it difficult for the country to treat chronic diseases like hypertension, diabetes mellitus, and hyperlipidemia. Increasingly, non-communicable diseases form the major burden of disease in the DPRK. WHO recently reported that 79% of deaths were caused by non-communicable diseases, of which 36% were due to cardiovascular disease and 17% due to cancer.[28] The household doctor system in the DPRK, which is a strong public network of primary healthcare, can support a vaccination or quarantine program for communicable disease relatively well, but quality care of non-communicable diseases cannot be optimized under the growing unofficial health market and increased disparity in healthcare access in the DPRK.
Photo 1: Pyongyang, North Korea – Lab at Maternity Hospital (Stephan via Flickr)

Trends in Global Health Aid to the DPRK during the International Sanctions Regime and the Role of the ROK Government in the COVID-19 Pandemic Era
Following the recent advent of COVID-19, the importance of health security – which is directly connected to infectious diseases – has received worldwide attention. Health security is also an important consideration in budget allocation for international development aid. The Global Health Initiatives (GHIs), which were formed to achieve the UN Millennium Development Goals in the early 2000s,[29] are mostly related to infectious diseases. One of them is GAVI, which is in charge of vaccination and immunization of infectious diseases, and another is the Global Fund[30] in charge of tackling tuberculosis, malaria, and AIDS.[31]
Health security is even more important to the DPRK, since it is directly related to the stability of the regime. Global healthcare assistance is a major channel for medical resources from the global community, and this has made the DPRK increasingly dependent on healthcare funds from multilateral organizations such as the Global Fund and GAVI.[32]
There are two primary features of these Global Health Initiatives. First, they strictly separate the phase of donor-state fundraising and the phase of partner state support provision. This means that the ROK, for example, cannot earmark donations to GAVI for the vaccination of infant children in the DPRK. In other words, these organizations first raise no-purpose-attached funds from donor states and then perform internal reviews and assessments to set up independent plans for sending aid to various partner states. That is why certain entities like the Inter-Korean Cooperation Fund from the ROK Ministry of Unification cannot send aid to the DPRK via GAVI or the Global Fund. Instead, the ROK funds GAVI and the Global Fund through the Ministry of Foreign Affairs’ Global Disease Eradication Fund, which is collected by taking about one dollar from each international flight reservation booked and purchased by an ROK citizen. The ROK Ministry of Foreign Affairs used these funds to donate around US$4 million to GAVI and the Global Fund yearly until 2018.
Second, global health initiatives have used performance based financing (PBF) schemes for low and middle income countries.[33],[34],[35] This means that if the Global Health Initiative deems that the partner state is performing poorly – based on certain performance indices related to the project on tuberculosis, malaria, or AIDS – it may discontinue its support. Therefore, partner countries are subject to significant pressures in carrying out these projects.
These two organizations are taking on a significant role in tackling tuberculosis and malaria as well as providing vaccines to infants and children in the DPRK. However, a healthcare system that is excessively reliant on external multilateral organizations for funding is inevitably extremely sensitive to external changes. The Global Fund, which had provided a total of $102.5 million to DPRK since 2010, suspended its assistance to the DPRK tuberculosis and malaria project in June 2018,[36] and the DPRK has subsequently been facing a crisis in controlling tuberculosis. In 2017, Christoph Benn, the Director of External Relations at the Global Fund, told the ROK government that the country’s total amount of contribution to the Global Fund only amounts to one third of what the Global Fund has sent to DPRK as aid, indirectly calling for an increase of the ROK’s contribution. However, the ROK maintained its previous level of contribution in 2018, and the Global Fund decided to discontinue its assistance to the DPRK tuberculosis program, with the justification that the distribution and effectiveness of aid within the DPRK was uncertain, and that it was difficult to persuade its board of directors and donor states. After the ROK decided to double its contributions to the Global Fund starting from 2019, the Global Fund resumed its support for the DPRK’s tuberculosis and malaria programs in January 2020. This is a classic example of how a country that financially depends on certain external organizations in tackling infectious diseases can become extremely vulnerable to geopolitics and the political decisions of international actors. It also suggests that, as a donor, it is very important for the ROK to maintain its direct and indirect financial support in order to contribute to the DPRK’s health and medical care, including COVID-19 tests, treatments, and vaccines through various multilateral organizations in spite of difficulties in inter-Korean cooperation and the DPRK’s COVID-19 lockdown.
Finally, as non-communicable diseases form the major burden of disease in the DPRK, future official development assistance focused on health for the DPRK should also focus on strengthening the health system – especially in the area of sustainable health financing and maintenance of human resources in the public healthcare sector. In a situation where the UN sanctions regime and the COVID-19 lockdown are still in effect, the role of various sub-agencies of the ROK takes on a vital role in supporting various multilateral organizations to provide consistent support to the healthcare system of the DPRK. These agencies and organizations must strategically coordinate with each other to carry out their respective roles.
Photo 2: Pukchong Hospital – A mother with her child

Future Inter-Korean Biomedical Cluster Cooperation at the Demilitarized Zone (DMZ) or Border Area in the Post-Pandemic Era
As preparation for future inter-Korean exchanges and cooperation in the post-pandemic era, the DPRK and the ROK can achieve great synergy if they were to work together on establishing a joint national disease management system and building an inter-Korean Biomedical Cluster at the Demilitarized Zone (DMZ) or in the border area.
There have been several recent outbreaks of infectious diseases on the Korean Peninsula. The outbreaks of COVID-19[37], avian influenza[38], swine influenza, and African swine fever[39] have shown the dire need for the DPRK and the ROK to establish a joint health approach.[40] In the narrow DMZ strip of the Korean Peninsula, the two countries must closely engage with each other to manage various infectious diseases and set up a joint quarantine system. The Disease Control and Prevention Agencies of the ROK and the DPRK are needed to set up a joint national disease management system, using their respective institutional strengths to set up a comprehensive joint quarantine system not only for humans, but also animals and plants.
Alongside traditional forms of one-way support, the DPRK and the ROK should build a sustainable and synergistic horizontal inter-Korean cooperation model in the post-pandemic era. We performed a broad literature review about the establishment of a joint biomedical cluster between two countries in a border region. One of the most prominent cases of a biomedical cluster is the Medicon Valley in Sweden and Demark.[41] Due to an economic crisis in early 1980, the two fellow Scandinavian countries decided to join hands to reduce the high unemployment rate in Sweden and high wage problems in Denmark. They did this by constructing a bridge across the sea between them and by setting up a joint cluster close to the border, which later became the Medicon Valley biomedical cluster. Today, Medicon Valley offers jobs to the Swedish people and an incentive for competition among businesses in Denmark. This benefits both countries and has become a model case of a cross-boundary biomedical cluster.
Similarly, the DPRK and ROK could establish a biomedical cluster for mutual economic benefit. It could become a great start for resolving problems related to health and food security, as well as sustainable economic development. In one recent study supported by the Korean Ministry of Unification, the authors suggest establishing an inter-Korean biomedical cluster that encompasses R&D, clinical activities, and industrialization near the border region between the DPRK and the ROK (Figure 2).[42]
Figure 2. The Blueprint of Inter-Korean Biomedical Cluster at the Demilitarized Zone (DMZ) or border area
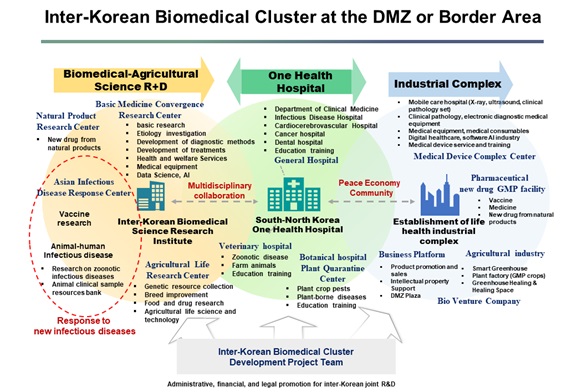
With regards to R&D, the cluster would take charge of convergent research on basic medicine, the study of natural products, prevention of infectious diseases, study on vaccines, study on animal diseases, and study on bio-agriculture. The DPRK has specialized in its own field of Korean medicine – Koryo medicine – and has considerable experience and expertise in developing drugs derived from natural products. If this expertise could connect with the pharmaceutical industry in the ROK, the DPRK and the ROK might be able to work together to raise global competitiveness in the field of naturally derived drugs, carrying out joint R&D projects and even establishing a new industry. With regards to clinical activities, a “One Health” hospital could be comprised of general hospitals for humans, veterinary clinics, plant clinics, and quarantine centers. General hospitals can treat various human diseases, while veterinary clinics could become centers for study of the African swine fever and other diseases that affect both humans and animals. Plant clinics could deal with pests that pose a threat to food security.
With regards to industry, the center would be tasked with raising bio-venture startups for developing and manufacturing medical equipment with the help of technology appropriate for a developing country, new drugs, and the bio-agriculture industry. It would also serve as a platform for new industries and markets. Software and artificial intelligence developers could cooperate on developing digital healthcare systems. In addition, the two Koreas could engage in joint R&D projects to develop vaccines and other essential drugs at the industrial complex. The bio-agricultural sector is also an important aspect of this cluster. A smart farming system should be developed in order to cultivate, manage, and harvest natural products for new drugs. Setting up a bio-agricultural complex would not only allow the production of plants for natural medicine, but also help the DPRK manage its food security through the bio-agricultural complex.
If an inter-Korean biomedical cluster could be established, it would become an effective model through which the DPRK and the ROK could mutually benefit. This biomedical cluster should be located where North and South Korean staff can freely commute within controllable boundaries. The DMZ would be the best place to start. The ROK’s sector and the DPRK’s sector can be connected by a “DMZ Peace Bridge” to allow a limited form of free exchange of staff and cooperation within a loop-shaped structure. If building the inter-Korean biomedical cluster in the DMZ is too difficult, then other bordering areas can be considered for the construction of airport-like structures on each side of the DMZ, where staff can go through a special entry system to process immigration procedures and move by trams to get to the other side.
Conclusion
This paper has covered three topics: 1) the impact of the COVID-19 lockdown and the international sanctions regime on the DPRK healthcare system, 2) trends in global health aid for DPRK and the role of ROK in the COVID-19 pandemic era, and 3) a future inter-Korean biomedical cluster cooperation model in the post-pandemic era.
Like other post-socialist countries, chronic under-funding of the healthcare sector, lack of financial support for healthcare providers, and loosening governmental control over them might lead to the emergence of an unofficial healthcare market in the DPRK. Deepening marketization of healthcare practices and the inequality of healthcare access seems to have been exacerbated in the DPRK, especially during the COVID pandemic crisis. Although the DPRK household doctor system forms a strong public network of primary healthcare and could support a national vaccination or quarantine program, it cannot optimize the quality of care for non-communicable diseases.
The DPRK has become increasingly dependent on healthcare funds through channels such as the Global Fund and GAVI, which work with health security and control specific infectious diseases. The Global Fund’s decision to discontinue its assistance for DPRK’s tuberculosis program in 2018 and the resumption of its support in 2020 showed that financial dependency on external organizations in tackling national infectious diseases leaves the DPRK vulnerable to international relations and political decisions. The ROK’s sustained financial support for the DPRK’s essential healthcare through various channels is important for maintaining the basic health of the DPRK people, in spite of difficulties in inter-Korean cooperation and the DPRK’s prolonged lockdown.
Finally, to build a sustainable and synergistic horizontal inter-Korean cooperation model in the post-pandemic era, an inter-Korean biomedical cluster at the DMZ or border area – which encompasses the vertical axis of humans, animals, and plants, and the horizontal axis of R&D, clinical activities, and industry – is a promising model for achieving synergy between the DPRK and the ROK. What would happen if the inter-Korean biomedical cluster does become a reality? First, the DMZ would no longer remain a symbol of the Korean war, but a symbol of life and peacebuilding. Also, the DPRK and the ROK can work together to address infectious diseases and other threats to health security on the Korean Peninsula, which could speed up the growth of a next-generation bio-industry. Moreover, they could build a model of coexistence in which research, clinical care, education, and production are intertwined in an interdisciplinary network. This network would be based on a model of economic cooperation that builds upon the notion of “One Health”, which encompasses humans, animals, plants, and the environment. The DPRK and the ROK should engage in horizontal cooperation, not one-way support, to lead a paradigm shift in technological cooperation on food and health security. Moreover, the economic benefits arising from the inter-Korean biomedical cluster could be used to tackle the spread of non-communicable diseases in the DPRK which would lower the price of peace on the Korean Peninsula, both in the short and long term.
III. ENDNOTES
[1] Shin, Y.-J., The DPRK’s COVID-19 Outbreak and Its Response. Journal for Peace and Nuclear Disarmament, 2021. 4(sup1): p. 320-341.
[2] Choi, E.M., COVID-19 vaccines for low- and middle-income countries. Trans R Soc Trop Med Hyg, 2021. 115(5): p. 447-456.
[3] Nichiporuk, B., COVID 19 and its labor demand, migration, and military force structure implications in East Asia. Journal for Peace and Nuclear Disarmament, 2021. 4(sup1): p. 308-319.
[4] Wouters, O.J., et al., Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. The Lancet, 2021.
[5] Nagi M. Shafik, C.Y.R., Kee B. Park. North Korea’s Vaccination Capabilities: Implications for a COVID-19 Campaign. 2021, AUGUST 5 [cited 2021 August 24th]; Available from: https://www.38north.org/2021/08/north-koreas-vaccination-capabilities-implications-for-a-COVID-19-campaign/.
[6] WHO, Evaluation of the Gavi Health Systems Strengthening Support to the Democratic People’s Republic of Korea. 2018.
[7] WHO, Global Health Workforce Statistics 2018. Geneva, WHO, 2018.
[8] Barrett, J., The North Korean Healthcare System: On the Fine Line Between Resilience and Vulnerability. Resilience: Interdisciplinary Perspectives on Social and Humanitarianism, 2011. 2: p. 52-65.
[9] Barrett, J., The North Korean Healthcare System: On the Fine Line Between Resilience and Vulnerability. Resilience: Interdisciplinary Perspectives on Science and Humanitarianism, 2011. 2: p. 52-65.
[10] Lee, H., et al., The role of major donors in health aid to the Democratic People’s Republic of Korea. J Prev Med Public Health, 2013. 46(3): p. 118-26.
[11] McCurry, J., North Korea’s health system in disarray. Lancet, 2010. 376(9738): p. 318.
[12] WHO, World health statistics 2010. 2010: World Health Organization.
[13] Analytica, O., North Korea’s economic catastrophe will only worsen. Emerald Expert Briefings, 2021(oxan-db).
[14] Andaya, E., The gift of health: socialist medical practice and shifting material and moral economies in post‐Soviet Cuba. Medical anthropology quarterly, 2009. 23(4): p. 357-374.
[15] Salmi, A.-M., Health in exchange: teachers, doctors, and the strength of informal practices in Russia. Culture, Medicine and Psychiatry, 2003. 27(2): p. 109-130.
[16] Park, Y.S., H.W. Lee, and S.M. Park, From Jeongseong to “Three-Minute Care”: Healthcare Transitions in North Korea and the Cultural Adjustment of North Korean Refugee Doctors in South Korea. Korea Journal, 2017. 57(4): p. 118-144.
[17] Park, S.M. and H.W. Lee, Current status of healthcare and effective health aid strategies in North Korea. Journal of the Korean Medical Association, 2013. 56(5): p. 368-374.
[18] Kyunghyo Chun, C.K., Sang Min Park, Haewon Lee, Recent Social Changes in North Korea, 2019. 2020, Seoul, Korea: Institute for Peace and Unification Studies
[19] Choi, Y.I., S.Y. Kim, and S.I. Hwang, [The influence of the devotion movement on the health care in North Korea]. Ui sahak, 2006. 15(1): p. 23-48.
[20] Frank, R., A socialist market economy in North Korea? Systemic Restrictions and a quantitative analysis. Systemic Restrictions and a Quantitative Analysis, 2003: p. 1-24.
[21] Ikpe, E., Challenging the discourse on fragile states. Conflict, Security & Development, 2007. 7(1): p. 85-124.
[22] Thresia, C., Rising private sector and falling ‘good health at low cost’: health challenges in China, Sri Lanka, and Indian state of Kerala. International Journal of Health Services, 2013. 43(1): p. 31-48.
[23] Grundy, J. and R. Moodie, An approach to health system strengthening in the Democratic Peoples Republic of Korea (North Korea). The International journal of health planning and management, 2009. 24(2): p. 113-129.
[24] Janes, C.R., et al., Poor medicine for poor people? Assessing the impact of neoliberal reform on health care equity in a post-socialist context. Global Public Health, 2006. 1(1): p. 5-30.
[25] Ferrinho, P., et al., Dual practice in the health sector: review of the evidence. Human resources for health, 2004. 2(1): p. 1-17.
[26] Jan, S., et al., Dual job holding by public sector health professionals in highly resource-constrained settings: problem or solution? Bulletin of the World Health Organization, 2005. 83: p. 771-776.
[27] García-Prado, A. and P. Gonzalez, Policy and regulatory responses to dual practice in the health sector. Health Policy, 2007. 84(2-3): p. 142-152.
[28] Park, J.J., et al., Systematic review of evidence on public health in the Democratic People’s Republic of Korea. BMJ global health, 2019. 4(2): p. e001133.
[29] Cometto, G., et al., A global fund for the health MDGs? The Lancet, 2009. 373(9674): p. 1500-1502.
[30] Brugha, R., M. Starling, and G. Walt, GAVI, the first steps: lessons for the Global Fund. The Lancet, 2002. 359(9304): p. 435-438.
[31] Ravishankar, N., et al., Financing of global health: tracking development assistance for health from 1990 to 2007. The Lancet, 2009. 373(9681): p. 2113-2124.
[32] Institute for Health and Unification Studies of Seoul National University, White Paper on Health and healthcare in North Korea. 2020, Seoul, Korea: Institute for Health and Unification Studies of Seoul National University.
[33] Fan, V.Y., et al., Performance-based financing at the Global Fund to Fight AIDS, Tuberculosis and Malaria: an analysis of grant ratings and funding, 2003–12. The Lancet Global Health, 2013. 1(3): p. e161-e168.
[34] Renmans, D., et al., Opening the ‘black box’of performance-based financing in low-and lower middle-income countries: a review of the literature. Health policy and planning, 2016. 31(9): p. 1297-1309.
[35] Bertone, M.P., et al., Performance-based financing in three humanitarian settings: principles and pragmatism. Confl Health, 2018. 12: p. 28.
[36] Park, K.B., U. Khan, and K. Seung, Open letter to The Global Fund about its decision to end DPRK grants. The Lancet, 2018. 391(10127): p. 1257.
[37] Ahmad, T. and J. Hui, One health approach and coronavirus disease 2019. Human vaccines & immunotherapeutics, 2020. 16(4): p. 931-932.
[38] Borland, S., et al., Influenza A virus infection in cats and dogs: a literature review in the light of the “one health” concept. Frontiers in public health, 2020. 8: p. 83.
[39] Kim, S.-H., et al., Wild boar harbouring African swine fever virus in the demilitarized zone in South Korea, 2019. Emerging microbes & infections, 2020. 9(1): p. 628-630.
[40] El Zowalaty, M.E. and J.D. Järhult, From SARS to COVID-19: A previously unknown SARS-related coronavirus (SARS-CoV-2) of pandemic potential infecting humans–Call for a One Health approach. One Health, 2020. 9: p. 100124.
[41] Frank, L., Biotechnology in the medicon valley. Nature Biotechnology, 2002. 20(5): p. 433-435.
[42] Institute for Health and Unification Studies of Seoul National University, The blueprint of inter-Korean biomedical cluster at the de-militarized zone (DMZ) or border area. 2020, Seoul, Korea: Institute for Health and Unification Studies of Seoul National University
IV. NAUTILUS INVITES YOUR RESPONSE
The Nautilus Asia Peace and Security Network invites your responses to this report. Please send responses to: nautilus@nautilus.org. Responses will be considered for redistribution to the network only if they include the author’s name, affiliation, and explicit consent


