DAVID LEGGE AND SUN KIM
OCTOBER 30 2020
I. INTRODUCTION
In this essay, David Legge and Sun Kim outline a policy platform to promote a more equitable roll out of vaccines in the context of the COVID-19 pandemic; and policy initiatives directed at a more equitable and efficient response to the next pandemic.
The essay may be downloaded in PDF format here
David Legge, MD, scholar emeritus at La Trobe University, has practised, researched and taught in public health, health policy and global health for many years. He has been active in the People’s Health Movement since its creation in 2000, including its WHO Watch project. Sun Kim, MS, PhD, Director of Health Policy Research Center at People’s Health Institute (Seoul, South Korea), has researched vulnerability and health care, and access to medicines and pharmaceutical production, from a political economy of health perspective. She has served as South East Asia and Pacific region coordinator of People’s Health Movement since 2019.
This essay is a working paper prepared for The 75th Anniversary Nagasaki Nuclear-Pandemic Nexus Scenario Project, October 31-November 1, and November 14-15, 2020, co-sponsored by Research Center for Nuclear Weapons Abolition, Nagasaki University (RECNA), the Nautilus Institute, Asia Pacific Leadership Network for Nuclear Non-proliferation and Disarmament.
Acknowledgement: Sun Kim acknowledges support by the Basic Science Research Program through the National Research Foundation of Korea (NRF) grant funded by the Ministry of Education (NRF-2017R1D1A1B03031898, Developing a ‘public’ pharmaceutical production and supply model for South Korea: historical and institutional contexts of pharmaceutical production and supply regimes in major countries).
The views expressed in this report do not necessarily reflect the official policy or position of the Nautilus Institute. Readers should note that Nautilus seeks a diversity of views and opinions on significant topics in order to identify common ground.
This report is published under a 4.0 International Creative Commons License the terms of which are found here.
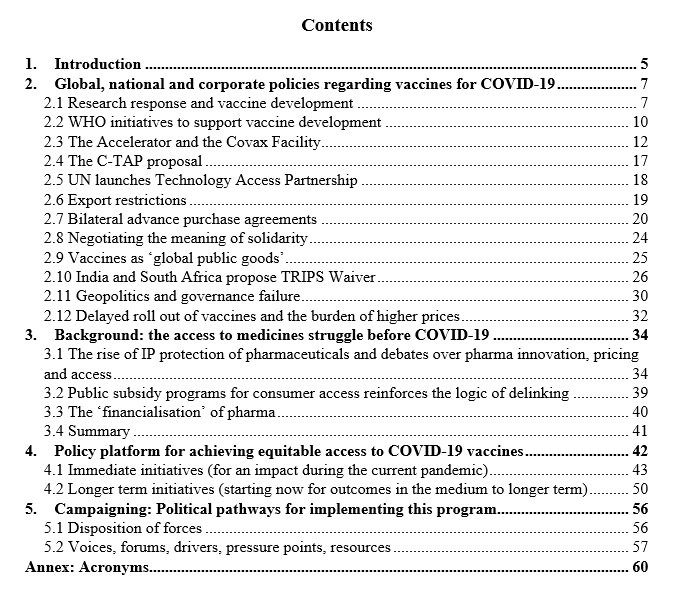
Banner image: Sophia Mauro for Nautilus Institute. This graphic shows the pandemic distribution from COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) on September 25, 2020; and the nuclear threat relationships between nuclear armed states.
II. NAPSNET SPECIAL REPORT BY DAVID LEGGE AND SUN KIM
EQUITABLE ACCESS TO COVID-19 VACCINES: COOPERATION AROUND RESEARCH AND PRODUCTION CAPACITY IS CRITICAL
OCTOBER 30 2020
Abstract
The COVID-19 pandemic has devastated families and communities and disrupted society and the economy; it has caused over 1 million deaths globally and left a disturbing burden of chronic morbidity. The prompt availability of effective and affordable vaccines against the SARS-2-coronavirus offers the most promising path out of the disease and disruption that the pandemic has wrought.
From the beginning the WHO Director General was emphasising ‘solidarity’ as the key to the global response. Solidarity was reflected in the early publication of the genome sequence and the sharing of protocols for the nucleic acid test. However, the proposal that vaccine technologies be pooled to accelerate vaccine development and production was a step too far for pharma and its nation state sponsors. WHO’s proposed ‘solidarity vaccine trial’ which would yield comparative data about efficacy, safety and cost was likewise boycotted by pharma.
From late March negotiations toward global cooperation for diagnostics, medicines and vaccines moved from WHO to the G20 sponsored ‘Access to COVID-19 Tools Accelerator’, a new ‘multi-stakeholder public private partnership’. The ‘vaccine arm’ of the Accelerator was the Covax Facility which would enter into advanced purchase commitments for selected candidate vaccines for participating countries. Covax also provided for the mobilising of donor funds to pay for vaccine supplies for low and lower middle income countries. Covax was designed to deliver vaccines for the priority fraction of countries’ populations (up to 20%). After this, countries would return to bilateral purchasing in the open market.
By July however, it was becoming clear that massive bilateral advanced purchase agreements, in particular, by the US, UK and EU, would reserve most of the early supply of effective vaccines and jeopardise the fund-raising for Covax.
The rejection of technology pooling, the rise of ‘vaccine nationalism’, and the underfunding (and under-supply) of Covax all look set to produce highly inequitable outcomes in terms of access to vaccination, particularly during the first year or so after the first vaccine is approved.
Drawing on a review of access-to-medicines debates over the last two decades, an analysis of the evolving business model of transnational pharma, and taking into account the rising call for universal health cover, we propose a policy platform to promote a more equitable roll out of vaccines in the context of the COVID-19 pandemic. Core elements of such a platform include:
- full funding of the concessional component of Covax;
- a rapid expansion of local production of vaccines in low and middle income countries (L&MICs) supported by an organised program of technology transfer as appropriate;
- an immediate waiver of key provisions of the TRIPS Agreement to facilitate access to intellectual property and technical knowhow necessary for vaccine development and production;
- full transparency regarding key aspects of vaccine development and production, including clinical trial data, production costs, and patent and market approval status; and
- a moratorium on national debt servicing and repayment for highly indebted L&MICs.
Policy initiatives directed at a more equitable and efficient response to the next pandemic need to be put in place now, including:
- scaling up public sector innovation and manufacturing capacity in L&MICs;
- regional and plurilateral agreements on biopharmaceutical technology transfer and capacity building;
- reforming the TRIPS Agreement to facilitate technology pooling in future pandemic emergencies;
- reforming the International Health Regulations to give WHO the power to trigger mandatory technology pooling and mandatory participation in comparative clinical trials (‘Solidarity trials’) in pandemic emergencies; and
- continued mobilisation around delinking and the creation of a global research and development treaty.
Critical to achieving progress in the implementation of this platform will be:
- institutional reform at the national level including legislation for the full deployment of TRIPS flexibilities and for the imposition of conditionalities on public funding of research (open licensing) and the funding of private pharma (transparency);
- protection of the multilateral member-state fora such the UN and the WHO where L&MIC voices can be heard and which can provide leadership in institutional reform; and
- community mobilization around single payer UHC and equitable access to affordable, effective medicines and vaccines.
COVID-19 has devastated families and communities and disrupted society and the economy. It has caused upwards of one million deaths globally[1] and left a disturbing burden of chronic morbidity[2],[3],[4]. The burden has fallen disproportionately on people in vulnerable groups[5] including people in residential aged care[6], health care workers[7], prisoners[8], oppressed racial groups[9],[10],[11],[12], other marginalised groups[13],[14] and low income people[15].
The public health measures deployed to contain the spread of the virus have impacted hugely on people’s lives, societal functioning and economic activity. Specific impacts include high levels of unemployment, disruption to the production of goods and services, bankruptcies, evictions, and family, corporate and government indebtedness. These social and economic impacts are not equally shared[16].
In many settings the health burden has been exacerbated by the economic burden. In the US (and other countries with employment related health insurance) the loss of jobs leads to the loss of health insurance and heightened barriers to seeking testing and treatment[17]. In countries without strong social security systems many low wage workers feel that they must continue to attend work (or go hungry), even when they are infectious, thereby increasing the risk of spread. Workers in precarious employment may continue to work in several different part time jobs, increasing their own exposure and the risk of spread.
A range of possible scenarios bringing longer term relief includes:
- the development of herd immunity through controlled spread;
- the development and widespread access to effective medical treatment, effective during the early phase of infection;
- development, production and widespread deployment of one or more vaccines;
- gradual amelioration of the virulence or infectivity of the virus.
Policy strategies which rely on controlled spread and the achievement of herd immunity may carry a heavy cost in terms of disease burden and even then appear unlikely to achieve the required levels of immunity[18].
At an early stage Sweden adopted a policy of moderate suppression, eschewing a more rigorous lockdown. By mid year it was evident[19] that Sweden had experienced a far greater mortality per capita (586 deaths per million at 24 October 2020 according to Worldometers) than its Nordic neighbours (Norway (51), Finland (64), Denmark (121)). However, it was still lower than some countries that opted for strict lockdowns, generally after an initial surge in cases, such as Britain (660), Spain (743) and Italy (618).
There has been a huge investment in finding medical treatments[20],[21],[22] but limited progress so far. Heparin[23], dexamethasone[24] and remdesivir[25] have all been shown to have a role in the treatment of very sick patients but there are no cures on the horizon. Even when effective treatments are found there will be significant challenges to deliver such treatments universally and equitably and the advent of effective treatments would not remove the need for restrictive public health measures.
The prospect of the pandemic receding through an amelioration of the virulence of the virus is highly speculative[26],[27]. Such a transition would take a long time and the burden would be heavy in the interim.
The development of one or more effective, acceptable and safe vaccine/s is the most promising of these possible scenarios. The outlook is promising on the technical front[28],[29],[30]. As of 19 October 2020 there were 44 vaccine candidates undergoing clinical evaluation and 154 in pre-clinical evaluation29. The candidate vaccines deploy a wide range of different technologies including several that have not previously been used in human vaccines. Some caution is called for in assessing the progress of the different vaccines; media coverage has been complicated by national interest posturing and company hype (directed to inflating the share price).
In the following section we review global, national and corporate policies regarding vaccine development and seek to locate them within the wider geopolitics of global governance. Against this background we assess the prospects for early equitable access to effective and affordable vaccines.
In Section 3 we review global debates over access to medicines since the signing of the Trade Related Aspects of Intellectual Property Rights (TRIPS) Agreement in 1994. This review of policy debate also serves to map the interests, institutions, organisations and forces within which equitable access to COVID-19 vaccines is being determined.
In Section 4 we set out a ‘policy platform’ for achieving equitable access to COVID-19 vaccines. We set out a program for immediate action during the COVID-19 pandemic and also sketch a range of longer term initiatives directed to the next pandemic. Finally, in Section 5 we explore political pathways for progressing this policy platform.
2. Global, national and corporate policies regarding vaccines for COVID-19
The purpose of this section is to review policy actions around access to vaccines which have been undertaken since the onset of the pandemic. This survey is necessary in order to estimate the prospects for an equitable and affordable roll out of effective vaccines as they become available. We explain why we think such prospects are dim.
2.1 Research response and vaccine development
A notice regarding an outbreak of a pneumonia of unknown origin was circulated by the Wuhan Municipal Health Committee on 30 December 2019[31]. (The earliest case among the first cohort of 41 cases studied by the Wuhan epidemiologists became sick on 1 December.) WHO was notified on 31 December 2019. By 8 January 2020 the agent had been identified as a coronavirus and its genome sequenced[32]. The genome was published on 11 January[33] and the first test to be endorsed by WHO (developed at Charité, Berlin) was announced on 13 January[34].
By late January, vaccine laboratories from around the world were reorienting their programs to focus on developing a vaccine for the new coronavirus. Pharmaceutical companies were activating their in-house research capacities and exploring possible relationships with laboratory research centres.
The Coalition for Epidemic Preparedness Innovations (CEPI) was well placed to act early. CEPI had been set up in 2016 following the 2014 Ebola crisis. It was funded and co-sponsored by the Gates Foundation, the Wellcome Trust and the governments of India and Norway[35]. CEPI already had a funding relationship with Inovio and the University of Queensland group and on 23 January announced new initiatives for a COVID-19 vaccine with these existing partners and with the US National Institute of Allergy and Infectious Diseases (NIAID)-Moderna partnership[36].
In late April 2020, CEPI and Gavi, the Vaccine Alliance, were assigned responsibility for the vaccines ‘pillar’ of the Access to COVID-19 Tools Accelerator (the ACT Accelerator, see below). CEPI dispenses ‘push funding’ in the form of grants to laboratories and vaccine companies; Gavi administers ‘pull funding’ through advanced purchase agreements and commitments via the Covax facility (more below).
While the Gates Foundation is a major funder of both Gavi and CEPI, it has also been independently working with many of the vaccine producers and laboratories. Bill Gates is believed to have played a significant role in dissuading the Oxford group from open licensing their technology[37] and instead partnering with AstraZeneca[38].
By August the role of CEPI and Gavi in funding vaccine development was over-shadowed by massive advance purchase agreements by the US, the UK and the EU for the most promising vaccine candidates (more below). While the UK and the EU were contributing to Covax as well as advanced purchasing, the US has not joined the ACT Accelerator but has invested hugely (in excess of $10 billion) in Operation Warp Speed.
Operation Warp Speed emerged out of a pre-existing network of US Government pandemic planners. These include Biomedical Advanced Research and Development Authority (BARDA), part of the HHS Office of the Assistant Secretary for Preparedness and Response and the Department of Defense Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense and the Army Contracting Command[39],[40].
In September the World Bank announced plans for a $12billion lending initiative to enable poor countries to purchase COVID-19 vaccines. The Bank acknowledged that it was responding to widely shared concerns that ‘vaccine nationalism’ (and the limits and underfunding of the Covax facility) would jeopardise access by L&MICs. “There has been substantial reservation of doses by the higher income countries and we want to make sure low and middle income countries have access as well,” the Bank President said[41].
The role of the military in supporting vaccine development in the USA appears to have been matched in both China[42] and Russia[43].
The prompt publication of the genome by Chinese scientists and the rapid development and sharing of nucleic acid tests by German, South Korean, and other researchers illustrate nicely the open source approach to the sharing of new technologies[44]. However, as the pandemic progressed and vaccine candidates emerged, the dominant approach became one of exclusive corporate ownership of the technologies and national hoarding of the products. WHO’s proposal for the ‘pooling’ of COVID-19-related technologies was derided by pharma executives[45] and dismissed by the governments of the USA, UK and Switzerland.[46]
The starkest illustration of the barriers created by the privatisation of vaccine technology was the refusal of vaccine manufacturers to participate in WHO’s comparative vaccine ‘solidarity’ trials.[47] Even now, with new vaccines being deployed in priority vaccination programs, there are no data available regarding the comparative efficacy, safety and cost of the different vaccines. CEPI’s new global laboratory network, announced in October[48] will compare vaccines’ immune responses but not their efficacy.
The contrast between the early open source approach and the later regime of privatisation and national hoarding is an important reference point for ongoing policy debates regarding technology pooling in the context of future pandemics.
2.2 WHO initiatives to support vaccine development
From early January WHO launched a range of initiatives directed to facilitating and targeting research and development. The roll out of these initiatives was informed by discussions at two global R&D forums; one in February[49] and one in July[50], both cosponsored by WHO and the Global Research Collaboration for Infectious Disease Preparedness (GloPID-R)[51]
WHO’s COVID-19 R&D Blueprint[52] was designed to facilitate a coordinated and accelerated response to COVID-19, including research towards an effective vaccine, research into potential treatments and strengthened channels for information sharing between researchers and countries.
Under the R&D Blueprint WHO developed a clinical trial protocol for a global, and globally coordinated, clinical trial for vaccines. The protocol envisaged a large, international, randomized controlled clinical trial (one of the proposed ‘solidarity trials’[53]) using a standardized study protocol that would enable the simultaneous evaluation of the benefits and risks of multiple candidate vaccines in sites with sufficient COVID-19 attack rates[54]. The radical benefit of the solidarity trial proposal was that it would yield comparative data regarding the efficacy of different vaccines[55],[56],[57]. It appears that there were no takers for the vaccine trial although the therapeutics solidarity trial did proceed and produced useful results[58].
WHO also convened a multidisciplinary working group to discuss and develop the concept of ‘human challenge’ studies68; deliberately infecting volunteers (immunised or not) with the coronavirus. The working group came up with eight criteria for approving human challenge studies[59]. The first human challenge trial was announced in London in late October[60].
WHO also developed a ‘target product profile’ for COVID-19 vaccines[61]. The document described the preferred and minimally acceptable profiles for human vaccines for long term protection of persons at high risk of COVID-19 infection, such as healthcare workers; and for reactive use in outbreak settings. Presumably regulators might refer to such a document in considering applications for marketing approval.
In addition to encouraging clinical trials (of medicines and vaccines) WHO also urged clinical trial sponsors to register such trials on its International Clinical Trials Registry Platform[62]. “The registration of all interventional trials is a scientific, ethical and moral responsibility.” Notwithstanding such urging it appears that failure to register has been common. A report by Health Action International and TranspariMED in August 2020[63] revealed a widespread failure of clinical trial sponsors in the Netherlands to meet their obligations to publish the results of their research.
In June WHO announced its ‘global framework to ensure equitable and fair allocation of COVID-19 products’[64], including global access principles, a global allocation framework, and fair and equitable allocation mechanisms (tailored for each intervention, starting with vaccines).
The global framework was based on an estimate that the priority fraction of countries’ populations at just over 20%. This was based on estimates for three population groups identified as key priorities for initial vaccination:
- Health care system workers (perhaps 1% of the global population, 50 million),
- Adults >65 years (8% of global population, 650 m), and
- Other high risk adults, with comorbidities (15%, 1,150 m).
The 20% figure was then used in the conception of the Covax Facility, designed to facilitate access to the priority 20%.
The framework has been criticised by academics[65] and some member states[66] as inherently favouring rich countries and failing to respond to the vulnerabilities associated with gender and poverty. Certainly, it failed to recognize the need to prioritise low income families in crowded housing or workers who could not afford to not go to work.
Other approaches to national allocation policies[67],[68],[69] have been published and in some cases modelled. Hogan and colleagues[70] comment that priority groups might vary according to vaccine supply. Their model suggests that priority should be given to the elderly if supplies are limited but as more doses come available the focus should be on interrupting transmission by vaccinating working aged people and perhaps children.
Chinazzi and Vespignani have modelled different scenarios for global allocation of limited vaccine supplies[71]. They conclude that if rich countries are able to monopolize COVID-19 vaccines, the global death toll could be twice as high as it would be if they were distributed more equitably.
WHO has deployed to the full the capabilities available to it through its constitution and funding. These include: convening (the two global fora), developing ‘normative’ products (the ‘unity study’ protocols, the allocation framework, the human challenge criteria), facilitating (the proposed ‘solidarity’ vaccine trial), and coordinating (the clinical trials registry).
2.3 The Accelerator and the Covax Facility
The Access to COVID-19 Tools Accelerator, launched at the end of April 2020[72],[73], describes itself as “a global collaboration to accelerate the development, production and equitable access to new COVID-19 diagnostics, therapeutics and vaccines”. It is sponsored by the Bill and Melinda Gates Foundation (BMGF), the Consortium for Epidemic Preparedness Innovations (CEPI), Gavi, the Global Fund, UNITAID, the Wellcome Trust, WHO, the International Red Cross and Red Crescent Movement (IFRC), the International Federation of Pharmaceutical Manufacturers (IFPMA), the Developing Countries Vaccine Manufacturers’ Network (DCVMN)[74], and the International Generic and Biosimilar Medicines Association (IGBA)[75],[76]. As of August 2020, US$3.8 billion had been pledged, out of the target figure of US $31.3 billion[77],[78],[79]. A further $1 billion was committed in a pledging session at the UN in late September[80].
The Accelerator has four pillars, dealing respectively with diagnostics, therapeutics, vaccines, and health systems.
The vaccines pillar builds on CEPI’s involvement in vaccine development and manufacturing and Gavi’s long-standing involvement in vaccine procurement and delivery in low income country settings. The objective of the pillar is “to ensure that vaccines are developed as rapidly as possible, manufactured at the right volumes without compromising on safety and delivered to those that need them most”[81].
The pillar plans to deliver 2 billion doses by the end of 2021, at a cost of US$18.1 billion, assuming a safe and effective vaccine is developed in the near future. An additional, 950 million doses would be procured by self-financing high-income countries and upper middle-income countries through the Covax Facility.
According to Gavi’s press release[82], Covax is “a new innovative financing instrument to provide access to COVID-19 vaccines for low- and middle-income countries” with the aim of establishing a “global mechanism to ensure equitable access to future COVID-19 vaccines.” Fifteen donors provided initial seed funding of just over $US500 million; the goal is to raise $US 2 billion[83],[84],[85],[86]. China and the Republic of Korea joined Covax in early October[87],[88]
The governance of Covax rests largely with Gavi and CEPI (and the Gates Foundation which funds both of them), while WHO is reduced to a marginal role and civil society is completely excluded.
Gavi explains that the Covax Facility is “a risk-sharing mechanism – reducing risk for countries concerned about failing to secure access to a viable vaccine and reducing risk for manufacturers concerned about investing without assured demand”88. Seth Berkley (GAVI CEO) said, “The worry we have is that unless we scale up production dramatically right now, and do that at risk, when the vaccines are available, they could be bought up by wealthy countries”[89].
The Covax Facility comprises two sets of advanced purchase agreements (APAs): one set of agreements between Gavi and the vaccine suppliers (perhaps 5-10 suppliers), and one set of APAs between Gavi and participating countries.
The agreement between Gavi and the vaccine supplier will specify a price and a total volume of doses. In sum the total volume of doses which Gavi agrees to buy, from all suppliers, will aim to cover up to 20% of the total population of participating countries (the priority fraction of those populations). It is understood that Gavi will only take delivery of vaccines that meet WHO standards with respect to efficacy and safety. There is no suggestion that participating suppliers will be required to return forward payments if their vaccine turns out to be ineffective or unsafe although they may get a bonus if they are successful.
The 20% figure adopted for Covax appears to have been based on WHO’s Equitable Allocation Framework although WHO’s calculations suggest a priority fraction of 24% (see above).
Two subsets of agreements will be struck between Gavi and participating countries; one for ‘self-funded countries’ (upper middle income (UMCs) and high income countries HICs)) and one for ‘funded countries’ (low income (LICs) and lower middle income countries (LMICs)).
The agreement with self-funded countries will specify a volume (based on doses needed to vaccinate up to 20% of total population for each country) and a price range (recognising that the agreed prices of the actually effective vaccines to be delivered may vary). Even though no country will receive enough doses to vaccinate more than 20% of its population until all countries in the financing group have been offered this amount, self-financing participants can request doses sufficient for up to 50% of their population, depending on the amount they pay into the Facility.[90]
The June 11 design document[91] indicates that vaccine suppliers will be asked to restrict their prices to “validated cost of production plus a small margin”. However, the document also notes that suppliers may insist on tiered pricing (differential prices according to countries’ ability to pay). The relationship between the price which is agreed between Gavi and the vaccine supplier and the price actually charged (and volume supplied) when supplies to individual countries are delivered is quite obscure at this stage (while Gavi knows what it is buying from a particular supplier; it has no way of knowing what it will be selling to participating countries). Self-funded countries will be required to pay a down payment, of around 10% of the total agreed purchase, up front.
The agreement between Gavi and the funded countries will specify a volume of doses calculated on an agreed minimum ‘high priority’ population which is likely to be well below the limit of 20% of the total population adopted for the self-funded countries. The cost of supply will be paid out of donations to the Covax facility. The volume and mix of vaccines provided to funded countries will be determined by Gavi.
It is understood that the Covax facility will only operate in the short to medium term and that, once participating countries have been supplied with the agreed doses for their ‘high priority’ populations, supply arrangements (prices, volumes and delivery dates) will revert to bilateral arrangements between individual countries (or purchasing consortia) and the vaccine suppliers[92]. It is also understood that individual countries (or purchasing consortia) may engage directly with vaccine suppliers even while they are participating in the Covax arrangements.
It is estimated that the proposed Covax Facility will require funding of up to USD 18.1 billion for the 2020/2021 vaccine supply. Of this total, USD 11.3 billion is sought urgently to cover investments in late 2020 including USD 2 billion in funding for advance market commitments to secure doses for low and middle income countries[93].
If everyone is to be vaccinated, the world will need 7.8 billion doses[94]. The Covax Facility needs 2 billion doses to ensure the 20% priority fraction of participating countries gets access. Covax has a $740 million deal with AstraZeneca for 300 million doses before end 2020[95]. It has a deal with the Serum Institute of India to produce 1 billion doses of the Oxford AstraZeneca vaccine for L&MICs including 400 million doses before end 2020[96]. It has deals (under discussion or finalised) with Moderna, Novavax, the University of Queensland, Clover, INOVIO, lnstitut Pasteur, University of Hong Kong, and CureVac[97]. The estimated total cost is $18 billion but the Facility is presently (late October) well short of that figure[98]. As bilateral advance purchase agreements ramp up competition to secure vaccine supplies will get even tighter.
In a recent addition to the Covax design, Gavi is planning for a Covax Exchange[99], where countries can trade vaccines doses earmarked for them. It appears designed to give the self-funded countries greater flexibility with a view to encouraging them to sign on. However, it may also contribute to greater inequity in distribution; HICs would not exchange entitlement to particular vaccines unless they are seeking to secure a better and/or cheaper vaccine. It is not clear whether vaccines earmarked for funded countries will be included in the exchange.
Assuming it is fully funded, and the suppliers have not committed all of their production to national deals, the Covax Facility promises some downwards pressure on prices, at least while supplies for the priority populations are being delivered.
However, this promise is quite uncertain as the massive bilateral advance purchase agreements (see below) are locking up projected vaccine supplies and exhausting national willingness to invest in Covax[100],[101]. Several European countries have already pulled out of the Covax Facility in favour of drawing on EU sponsored advance purchase agreements[102].
Any price benefits from participating in Covax will only extend to the first “20%”. After that the system reverts to bilateral purchasing with full price discretion for suppliers and no obligations regarding supplier transparency nor any obligation to factor in public subsidies (to research, development and production) in prices. The suppliers are likely to use tiered pricing from this point but the price levels and cut off points for such tiered pricing are quite opaque at this stage[103]. The ability to charge higher prices for rich countries will incentivize suppliers to prioritise rich countries in the early ‘post priority’ period when supplies are still limited. (AstraZeneca has pledged that it will not seek to make a profit from its vaccine until after the pandemic ends. However, the company appears to have reserved to itself the determination of when the pandemic ends[104].)
See Patnaik for a more detailed analysis of Covax governance[105].
The COVID-19 Technology Access Pool (C-TAP), endorsed by the World Health Assembly in May 2020[106], takes a very different approach.
The C-TAP[107],[108] is a ‘technology pool’ through which data, knowhow and intellectual property regarding existing or new COVID-19 health products will be pooled in order to accelerate the discovery of vaccines, medicines and other technologies through open-science research, and to fast-track product development by mobilizing additional manufacturing capacity. This will help ensure faster and more equitable access to existing and new COVID-19 health products.
There are five key elements to this ‘pooling’[109]: (i) public disclosure of gene sequences and data; (ii) transparency around the publication of all clinical trial results; (iii) governments and other funders are encouraged to include conditionality provisions clauses in funding agreements with pharmaceutical companies and other innovators specifying equitable distribution, affordability and the publication of trial data; (iv) licensing of potential treatments, diagnostics, vaccines or other health technologies to the Medicines Patent Pool; and (v) promotion of open innovation models and technology transfer arrangements that increase local manufacturing and supply capacity, including through joining the Open COVID-19 Pledge and the Technology Access Partnership (TAP).
WHO, Costa Rica and all the co-sponsor countries have also issued a “Solidarity Call to Action” asking relevant stakeholders to join and support the initiative, with recommended actions for key groups, such as governments, research and development funders, researchers, industry and civil society.
In a letter to the US Congress in March, in support of the Costa Rica initiative[110], James Love (Knowledge Ecology International, KEI) urged the US Government to expand access and increase the supply of products by buying out patent and data rights, and/or offer incentives like innovation inducement prices and market entry rewards to delink the incentives for development from the grants of legal monopolies.
As of late May, the C-TAP was supported by the 34 L&MICs and a small number of European countries[111]. The UK and USA have shown no interest in supporting C-TAP[112]. Civil society commentary on C-TAP has varied between support and criticism, the latter generally based on the voluntary nature of the proposal. The chief executive of Pfizer described the pool as ‘nonsense’ and ‘dangerous’ with similar disparagement from the CEO of AstraZeneca[113],[114]. The threat for pharma is that it might open the door to more widespread open licensing[115].
In July 2020, the European Parliament adopted a resolution proposing a European Health Union and the establishment of a European Health Response Mechanism[116],[117]. This resolution contains strong language in support of C-TAP, de-linkage mechanisms, transparency, and compulsory licensing. The resolution envisages the use of compulsory licensing in the event that third countries (non-EU member states) do not share COVID-19 vaccines, therapeutics and know-how.
C-TAP would be an appropriate platform to realize the pooling of technology and knowledge as ‘global public goods.’ However, so far it has failed to achieve such pooling due to the low participation from the major countries and the TNCs with IP. It needs more realistic rewards and penalties, to compel pharma to join.
2.5 UN launches Technology Access Partnership
On May 12 2020, The United Nations Technology Bank, together with the UN Development Programme (UNDP), UN Conference on Trade and Development (UNCTAD), and the World Health Organization (WHO), launched the Technology Access Partnership (TAP) in a joint effort to scale up local production of health technologies in response to COVID-19. The TAP initiative is an extension of the long-time cooperation among the UNDP, UNCTAD, and WHO in support of local production in L&MICs.
It is a critical platform for equitable access to the health technologies in response to COVID-19 for L&MICs, with a combination of technology transfer and capacity building for R&D, production, and supply. However, at this stage, its scope is restricted to PPE, medical devices, and diagnostics[118],[119]. The exclusion of medicines and vaccines from its scope is perhaps a sign of the behind the scenes power of pharma to pre-empt international policy development. The scope of TAP needs to be expanded to include medicines and vaccines.
‘Beggar thy neighbour’ export restrictions have been a feature of the COVID-19 pandemic since the beginning. An information note produced by the WTO in April 2020[120] listed a wide range of export restrictions imposed by various countries to protect domestic supply often at the cost of other countries in greater need. Most of these export restrictions applied to medical supplies (e.g. facemasks and shields), pharmaceuticals and medical equipment (e.g. ventilators), but others have extended controls to additional products, such as foodstuffs and toilet paper.
The information available to WTO in late April suggested that 80 countries and territories had introduced export prohibitions or restrictions as a result of the COVID-19 pandemic, including 46 WTO members (72 if EU member states are counted individually) and eight non-WTO members. Most of these have been described as temporary measures. At least two members had removed some of those restrictions. WTO noted a lack of transparency regarding these restrictions.
The Republic of Korea (South Korea) imposed export restrictions on face masks in February 2020[121]. While ordinary Korean people wore KF-94 (similar with N-95) face masks outside on the street, health care personnel in Europe were exposed to COVID-19 infection due to lack of supply of face masks.
France and Germany imposed export restrictions on PPEs including face masks and respirators in March[122]. White House trade adviser Peter Navarro said at the time that “such behaviour is precisely why it is important for the Trump administration to bring home its manufacturing capabilities and supply chains for essential medicines and thereby simultaneously reduce America’s foreign dependencies, strengthen its public health industrial base, and defend our citizens, economy, and national security”[123].
In April, President Trump placed export restrictions on the N-95 respirators produced by 3M[124]. Canadian Prime Minister Justin Trudeau criticized Trump’s move[125] and 3M CEO warned that “ceasing all export of respirators produced in the United States would likely cause other countries to retaliate and do the same, as some have already done,” and “if that were to occur, the net number of respirators being made available to the United States would actually decrease.”[126].
Such behavior is likely to be repeated in vaccines. Given that the R&D and production capacity of vaccines is much more concentrated in some rich countries compared to the PPEs, the impact of export restrictions on unequal distribution will be greater.
Bollyky and Brown comment[127] that such hoarding is not new. “A vaccine was developed in just seven months for the 2009 pandemic of the influenza A virus H1N1, also known as swine flu, which killed as many as 284,000 people globally. But wealthy countries bought up virtually all the supplies of the vaccine. After the WHO appealed for donations, Australia, Canada, the United States, and six other countries agreed to share ten percent of their vaccines with poorer countries, but only after determining that their remaining supplies would be sufficient to meet domestic needs.”
The Serum Institute of India (SII) has a deal with Covax to produce 1 billion doses of the AZ vaccine for L&MICs including 400 m doses before end 2020[128]. SII also has a manufacturing deal with the Novavax[129]. SII CEO Adar Poonawalla said in an interview that “out of whatever I produce, 50% to India and 50% to the rest of the world”[130].
SK Bioscience from South Korea has manufacturing deals with AstraZeneca and Novavax. In parallel with these two deals, it has signed two trilateral letters of intent (LOI) with the Korean Ministry of Health and Welfare; one with the AstraZeneca and the other with the Novavax. Both LOIs included the same ‘three shared goals’: ensuring fast and stable production and export, strengthening production capacity to cope with demand, and securing domestic supply of the vaccine[131],[132].
2.7 Bilateral advance purchase agreements
Perhaps most significant in shaping the availability of vaccines has been the flurry of bilateral advanced purchase agreements (for vaccines which are yet to be shown to be efficacious). The volume of doses covered by such agreements clearly jeopardises the chance of other countries accessing such vaccines and jeopardises the success of the Covax initiative, both in terms of competing for public monies and in terms of the supply of doses. Oxfam calculated that by mid September that wealthy nations, representing just 13 percent of the world’s population had cornered more than half (51 percent) of the projected doses of leading COVID-19 vaccine candidates[133].
In terms of bilateral deals the US is the leading purchaser. As of late August the US had deals in place with seven companies securing at least 800 million doses and costing a total of $10 billion125,[134]. These include deals with AstraZeneca[135],[136], Novavax[137], Moderna[138], BioNT Pfizer[139],[140], and Sanofi-GSK[141].
The US has been the pioneer in terms of bilateral APA deals. On March 2, the White House invited 10 representatives of pharmaceutical companies developing COVID-19 vaccines to a meeting of the White House Coronavirus Task Force. Operation Warp Speed was announced in early April.
In May, the US government included a supply condition in its agreement to support AstraZeneca’s candidate vaccine. At least 300 million doses of the vaccine should be provided for the US, with the first doses should be delivered as early as October 2020. Since then, the US government attached similar supply conditions in its agreements for other companies including Novavax, Pfizer, GSK, J&J and Moderna[142]. These APAs will constrain the volume of doses available for Covax in the short to medium term.
The March 2 White House meeting triggered vaccine nationalism across the globe. On May 13, Paul Hudson, CEO of French company Sanofi, which had also been invited to the event, said in an interview that “the U.S. government has the right to the largest pre-order because it’s invested in taking the risk”[143]. The French President Macron said when he heard this that any vaccine against COVID-19 must be treated as “public good for the world, and not subject to the laws of the market”[144]. Two months later President Macron was insisting that France would be among the first countries to get access to a potential vaccine being developed by Sanofi[145].
The United Kingdom is the world’s highest per-capita buyer, with 340 million doses purchased: around 5 doses for each citizen[146]. UK aiming to secure deals for 12 vaccines. It has deals in place with: AstraZeneca[147],[148],[149], Moderna[150], BioNTech-Pfizer[151], Valneva143, and Sanofi GSK[152].
The European Commission approved spending of up to $2.6 billion on advance purchase agreements for vaccines in June[153]. Prior to that the European Inclusive Vaccine Alliance[154],[155] was driving European purchases. Deals now in place involve: AstraZeneca[156],[157],[158], Johnson & Johnson[159], and Sanofi-GSK (31/7)150.
The German government has taken a 23% share in CureVac[160] which presumably entails priority access, in addition to supplies procured through the EU. GSK also has a 10% stake in CureVac[161]. (In March the US was allegedly rebuffed by the German government when the Trump Administration allegedly sought to persuade CureVac to move to the US and grant to the US exclusive access to their vaccine[162],[163],[164],[165].)
UK, EU, Canada, and Japan are following both tracks: APAs for several vaccines with different platforms, in parallel with the participation in the Covax Facility[166]. The EU and Canada, which had been insisting on ‘global public goods’ against US dominance, eventually joined the competition by signing several APAs. Japan has deals in place with AstraZeneca[167], Pfizer and BioNTech[168] and with Novavax. Switzerland has a deal with Moderna[169].
The Government of Canada has entered into two agreements, with Pfizer and Moderna, to secure millions of doses of candidate vaccines. Pfizer will supply its BNT162 mRNA-based vaccine candidate, while Moderna will provide its mRNA-1273 vaccine candidate[170]. Canada is also dealing with Novavax and Johnson & Johnson[171].
Australia is negotiating with AstraZeneca (AZ) for 30 million doses, to be produced by CSL in Australia, for Australia, NZ and Pacific[172]. It has committed to supporting the Covax advanced market commitment for L&MICs in the Asia-Pacific region but has not committed to joining the Covax Facility to secure domestic supply.
India, through the SII and Biological E, has arrangements with Oxford-AstraZeneca, Novavax and Johnson&Johnson (J&J)[173]. Brazil has also joined in signing APA with AstraZeneca, “due to the global movement for mobilization and acquisition of vaccines”[174].
Both Russia and China are expecting to use domestically produced vaccines. Russia has signed an agreement with Kazakhstan, The Philippines and two Brazilian states to supply its vaccine. China is negotiating to supply its vaccines to its allies in the Asia Pacific region.
AstraZeneca is well ahead of other suppliers in advance purchase deals with over $2 billion booked. AstraZeneca is also putting in place manufacturing deals with vaccine manufacturers in India (SII), China (BioKangtai), Brazil (Fiocruz), and South Korea (SK Bioscience). Novavax also has a manufacturing deal with the SII and J&J has a corresponding deal with Biological E[175]. The details are different in each case – whether domestic supply is included or not, whether marketing license is included or not, whether technology transfer is included or not, whether the national government was involved in the agreement or not etc.
It is clear that bilateral advance purchase agreements will tie up a large proportion of approved vaccines for a considerable time. More critically in terms of equitable access, the financial commitment that rich countries are making to these bilateral purchases bodes poorly for the full funding of Covax. Likewise global production capacity will be tied up fulfilling bilateral purchases for a significant period.
2.8 Negotiating the meaning of solidarity
For countries which have secure supplies of promising candidate vaccines there is a logic to export restrictions, based on the obligation to the electorate to meet domestic needs. Against this imperative, solidarity with people in poorer countries comes a distant second. But what about after the priority fraction of the population has been vaccinated? WHO’s estimate of the priority fraction is somewhat rubbery and flawed in important respects, but we may take the figure of 20-25% of the population as a reasonable estimate of the size of the priority fraction.
Let us accept that those countries who have secured supplies through advance purchases will allocate doses to their priority fraction first. However, in terms of international solidarity we may ask, at what point will they pause in the domestic roll out to ensure that the priority fraction in L&MICs is also supplied? Will they continue to roll out domestic vaccination to 50% or to 80% before they pause and release their stockpiles?
These are choices which are made by governments but which are also dependent on public sentiment. If political leaders are leaning to solidarity will they have public support? If political leaders are leaning to prioritising the domestic roll out, at what point will public sentiment call for a pause?
In some degree, these are questions of national culture and the strength of solidarity versus self-interest. However, on top of inherited cultures, comes the celebration of individual self-interest as a driver of social development which has been a prominent theme of the neoliberal offensive over the last three decades. The rise of neoliberalism has also been accompanied by a widening of income inequality and existential insecurity. It is hard to express solidarity from the darkness of alienation and insecurity.
Since the COVID-19 pandemic emerged Dr Tedros has, on a daily basis, called for solidarity. However, there are limits to exhortation. The longer term need, in public health planning and across the broadest front of social policy, must involve challenging the naturalisation of inequality and insecurity.
2.9 Vaccines as ‘global public goods’
While ‘vaccine nationalism’ looms large, the arguments for technology pooling and a more equitable allocation of affordable vaccines have been advanced under the slogan of ‘global public goods’[176].
At the WHA in May Presidents Xi Jinping of China and Emmanuel Macron of France both referred to the development of a COVID-19 vaccine as a ‘global public good’. Likewise Germany’s Angela Merkel and South Africa’s Cyril Ramaphosa have also called for COVID-19 vaccines to be treated as ‘global public goods’.
When Presidents Carlos Alvarado Quesada of Costa Rica and Sebastián Piñera of Chile joined the WHO Director-General Dr Tedros on 15 May to announce the C-TAP technology access pool they promised that it would pool data, knowledge and intellectual property for existing or new COVID-19 health products to deliver ‘global public goods’ for all people and all countries.
Resolution WHA73.1[177],adopted in May 2020, calls for “universal, timely and equitable access to, and fair distribution of, all quality, safe, efficacious and affordable essential health technologies and products … required in the response to the COVID-19 pandemic as a global priority” and “the spirit of unity and solidarity, the intensification of cooperation and collaboration at all levels in order to contain and control the COVID-19 pandemic and mitigate its impact”.
During the UN discussion of the Omnibus COVID-19 resolution, Peru, Mexico, and Iran called for vaccines to be treated as global public goods.
On 14 May, a day before the WHO announced the C-TAP technology access pool, and before the 18 May WHA, Oxfam in collaboration with UNAIDS published the open letter signed by ‘world leaders’, entitled ‘the People’s Vaccine’. It describes the principle of it as (i) available to all, (ii) in all countries, and (iii) free of charge[178],[179].
In a June blog MSF Access[180] listed six recommendations to help ensure that future COVID-19 vaccines would be accessible for everyone who needs them. These included: (i) strings attached, (ii) at-cost pricing, (iii) transparency, (iv) deciding together, (v) equity, and (vi) global public good.
On 23rd June 2020, 45 civil society organizations sent a letter to the board members of Gavi highlighting various concerns with the Covax proposal[181]. They argued that the initiative demonstrated that Gavi and governments were not delivering on the promise of designating COVID-19 vaccines as ‘global public goods’, adding that in a “business as usual” approach to intellectual property, “pharmaceutical companies are allowed to retain and pursue rights to vaccines under development, resulting in vaccines that are proprietary and under the monopoly control of individual companies.
The June 2020 Civil Society Letter to members of the GAVI Board[182] likewise highlights seven key points: (i) vaccines must be allocated based upon public health criteria for all countries; (ii) transparency must be fundamental to the Covax Facility; (iii) prices must be set ‘at-cost’; (iv) no risky advance payments without clear conditions; (v) operate in line with WHO’s Solidarity Call to Action for equitable global access to COVID-19 health technologies; (vi)non-governmental purchasers must be included; and (vii) accountability is critical.
2.10 India and South Africa propose TRIPS Waiver
Many developing countries have expressed serious concerns over the barriers imposed by the TRIPS Agreement on affordable access to diagnostics, vaccines and therapeutics that are being currently developed for combating the COVID-19 pandemic, as well as the so-called “vaccine nationalism” already occurring even before clinical trials have concluded. Seven months into the pandemic, these growing concerns culminated in a proposal by India and South Africa for a waiver for a range of intellectual property rights provided for in the TRIPS Agreement for COVID-19 products until a vaccine is widely available.
South Africa, in particular, had raised concerns about the TRIPS Agreement as early as June. Officials from South Africa repeatedly highlighted[183],[184],[185] the importance of TRIPS flexibilities in facilitating access to medical products which might otherwise be not available or affordable. At an informal meeting of the TRIPS Ministerial Council in June[186],[187] South Africa pointed to the barriers that many developing countries face in using TRIPS flexibilities. South Africa also highlighted the inadequacies of the provisions in the TRIPS Agreement for compulsory licensing for export (so that countries without local manufacturing can access the benefits of compulsory licensing in the COVID-19 response). At a meeting in July, sponsored by the Africa Union, African health ministers also underlined their concern that patents and other technology barriers could negatively impact the ability of developing countries to access future COVID-19 vaccines[188].
Ideas for strategies to overcome the barriers created by TRIPS had already been circulating in civil society forums. In a webinar in May, organised by the South Centre[189], Dr Carlos Correa discussed how IP can create barriers to affordable access and discussed the various instruments that governments can use legitimately to overcome these, including through the non-grant of secondary medical use patents and application of rigorous standards in the examination of patent applications. Other instruments cited included compulsory licensing and the use of the security exception under Article 73(b) of the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS). Dr. Correa also discussed proposals for a moratorium on TRIPS obligations and the pooling of IP-protected technologies, know-how and data. He pointed out that these instruments are not mutually exclusive and all options should be on the table.
On 2 October India and South Africa communicated to the WTO TRIPS Council a proposal for a waiver of certain provisions of the TRIPS Agreement[190]. India and South Africa referred to reports about IPRs hindering or potentially hindering timely provisioning of affordable medical products to patients. In particular, they cited the cumbersome and lengthy process for the import and export of pharmaceutical products under the requirements of Article 31bis. They requested that the TRIPS Council endorse a waiver of sections 1, 4, 5, and 7 of Part II of the TRIPS Agreement, in relation to COVID-19; to remain in place until widespread vaccination is in place globally, and the majority of the world’s population has developed immunity. Section 1 of part II of the TRIPS Agreement pertains to copyright and related rights; section 4 deals with industrial designs. Section 5 of part II of the TRIPS Agreement pertains to patents; section 7 deals with the protection of undisclosed information.
There was widespread civil society support for the waiver proposal. A sign on letter sponsored by the Third World Network attracted over 400 signatories from around the world[191]. The letter assembles comprehensively the case for the waiver, referring to the refusal of the pharmaceutical companies to participate in WHO’s C-TAP, the use of secretive and restrictive licensing agreements, commercial disputes regarding alleged IP infringements in relation to COVID-19 products and global shortages. The letter acknowledged the possibility of deploying TRIPS flexibilities but pointed out that, “compulsory license offers a “product by product”, and “country by country” approach with variations in national laws, whereas the pandemic requires collective global action to tackle IP barriers and facilitate technology transfer”. It also noted the clumsy requirements of Article 31bis in issuing compulsory licenses for export/import.
MSF circulated a detailed briefing paper[192] which included an overview of the impact of IP barriers on access to therapeutics, vaccines and diagnostics; three case studies examining IP barriers in the context of COVID-19 and examples of Article IX waivers that have been granted with respect to provisions under the Trade-Related Aspects of Intellectual Property Rights Agreement (TRIPS) Agreement in the past.
The proposed waiver was also supported by UNAIDS[193], UNITAID[194] and WHO’s Director General Dr Tedros[195].
Soon after the India and South Africa proposal was tabled, the WTO Secretariat pulled together an ‘information note’ on the TRIPS Agreement and COVID-19[196], apparently designed to cut across the waiver proposal and to provide arguments for countries opposing.
When the proposal was opened at the TRIPS Council meeting on 16 October it was supported by a number of developing countries including China[197],[198] but opposed by several wealthy countries (plus Brazil). The proposal was suspended with the expectation of it being reviewed in a further meeting later this year[199],[200].
Three main arguments were brought forward in opposition to the waiver: that IP protection is not a barrier to wider access to COVID-19 health products; that the flexibilities provided for in the TRIPS Agreement are adequate; and that IP is necessary to fund innovation[201]. See for example the UK statement[202].
It is true that there are a range of barriers to be overcome in the development of diagnostics, treatments and vaccines, many of which are not related to IP. However, there are several examples that demonstrate that IP ban be a significant barrier it is also true that IP disputes have created barriers to scaling up vaccine production in the US[203] and that the voluntary licenses imposed by AstraZeneca on the Serum Institute of India include arbitrary restrictions on countries to whom vaccines can be sold[204].
The argument that IPRs are necessary to fund innovation is hardly consistent with the dependence of current R&D on donor funding and advance purchase agreements.
The proposition put forward by opponents of the waiver that the flexibilities provided for in the TRIPS Agreement are adequate is extremely cynical in view of the big power bullying of L&MICs by the EU and the US regarding legislating for and using such flexibilities[205]. As was pointed out in the CSOs letter, organized by TWN, TRIPS flexibilities are not sufficient for the present pandemic situation. Compulsory licensing provides a “product by product”, and “country by country” approach whereas the pandemic requires collective global action to facilitate technology transfer and scale up manufacturing more broadly.
It is important to be clear about the differences between the proposed waiver, the existing TRIPS flexibilities (where they have been domestically legislated), WHO’s C-TAP initiative, MSF’s campaign to not give patents to COVID-19 diagnostics, treatments or vaccines[206], or the Open COVID-19 Pledge[207], which would allow voluntary use (open licensing) of all patents and other intellectual property rights. The waiver would suspend the protections provided under TRIPS for copyright, industrial designs, patents and technical knowledge. These protections ultimately depend on state to state dispute settlement. Access to such technologies might still be illegal under domestic law. Alternatively, where TRIPS flexibilities have been incorporated into domestic law, access to such technologies could still be facilitated through compulsory licensing, parallel importing or other mechanisms.
There is also a certain logic in collective action by L&MICs through a TRIPS waiver, given the aggressiveness of US and European sanctions on individual countries who seek to legislate for the full use of TRIPS flexibilities and to actually use them. A group of South African academics wrote to President Ramaphosa in the lead up to the TRIPS Council meeting congratulating him on the Indian and South African initiative[208] but urging him to act regionally and nationally as well as globally. However, he may have judged that he would be less exposed to sanctions if the waiver proposal was adopted than if South Africa were to act unilaterally. That said, the opposition to the waiver in the WTO was predictable. While the proponents could still find the 75% of members required to agree to the waiver[209], the significance of the campaign may ultimately arise from its salience in the longer term struggles against extreme intellectual property laws more generally.
If the waiver campaign was in part directed at challenging the legitimacy of the TRIPS and TRIPS Plus regimes it appears to have been heard at Moderna which on October 8 pledged not to enforce its patents[210] during the pandemic. Moderna’s initiative was warmly received by KEI[211], less so by Health GAP[212].
2.11 Geopolitics and governance failure
Ongoing debates regarding access to medicines have focused largely on technical details such as the specific provisions of intellectual property law and the cost of innovation and production. However, the wider geopolitical context of these debates must also be considered. Resistance to ideas such as delinking and an R&D treaty is rooted deeply within the structures and ideologies of transnational capitalism in the era of neoliberalism.
The evolving dynamics of global political economy have also framed the successes and failures of global governance during the COVID-19 pandemic.
The UK, US and Switzerland dismissed the proposed COVID-19 Technology Access Pool from its inception and none of the governments hosting vaccine developers have required that ‘their’ vaccine developers participate in WHO’s proposed solidarity trial. While most OECD governments are participating in the Accelerator and the Covax Facility the US is participating in neither.
The HIC governments have generally supported the privatisation of vaccine technologies, notwithstanding the barriers arising therefrom to local production in L&MICs. The support of HICs for privatisation of vaccine technologies has been defended on the grounds that profits from monopoly pricing are necessary to incentivise innovation. This is clearly hollow in view of the long-standing reluctance of pharma to invest in vaccine development without public funding. The privatisation of vaccine technologies is deeply rooted in the dynamics of transnational capitalism, including the role of intellectual property in maintaining the asymmetric economic relationships between HICs and L&MICs, and the role of transnational corporations in mediating these relationships.
On April 15, President Trump declared a halt to US funding of the WHO, and on May 29 officially notified the WHO of the US withdrawal[213]. Whether President Trump (assuming he is re-elected) has the constitutional power to withdraw from WHO without Congressional support is moot[214]. The loss of US funding would weaken WHO in the short term; the removal of the US insistence on the freeze on assessed contributions could benefit WHO in the medium to longer term.
The hostility of the Trump Administration to multilateralism (including the WTO as well as WHO) resonates with Trump’s domestic constituency who perceive that they have been betrayed by the globalisation project, including, in particular, by the off-shoring of decent jobs; replaced by the precarious and low wage ‘gig economy’. The new Cold War against China plays to a resentment in the Trump base regarding China’s economic development, which is seen to have been facilitated by globalisation, driven by the transnational fraction of US capital.
A similar interplay between domestic politics and international relations is evident in the priority given (by the UK, Europe and the US) to advanced purchase agreements, while providing little more than token support to the Covax Facility (no support in the case of the US). Governments are caught between being blamed by their people for recurring waves of the COVID-19 epidemic while confronting resistance to the COVID-19 lockdown. Betting on vaccines is a response to both.
Failures of governance at the national level may also reflect contradictions associated with the neoliberal ascendancy which has accompanied and facilitated the globalisation of transnational capitalism. Widening inequality and deepening insecurity, both of which have been driven and rationalised by neoliberal ideology, have contributed to lockdown resistance which in turn has contributed to the failures of epidemic control. In settings with minimal safety nets it can be difficult, even infuriating to be faced with a choice between lockdown compliance (when it threatens dispossession, indebtedness, and even hunger) versus resistance. The neoliberal prescriptions of deregulation, privatisation and small government may have also contributed to failures in COVID-19 control.
Stiglitz and Rashid point out[215] that “developing economies are facing a severe debt crisis, exacerbated by the COVID-19 pandemic. If no action is taken to avoid a debt crisis in the developing world, the long-term effects on their public spending, employment and economic development will be staggering”. Sovereign debt owed to private creditors increased nearly three-fold during the past decade, from $186 billion in 2008 to $535 billion in 2018. Nearly 90% of this is sovereign bonds.
Global Citizen[216] has called for a suspension of debt so that poor countries can respond to the pandemic. They note that the G20, has already agreed to suspend debt for the poorest countries. “However, this doesn’t cover debt held with private creditors — including big banks and hedge funds — to whom the poorest countries will otherwise have to repay a shocking $16 billion in 2021. This amount could buy over 3 billion COVID-19 tests.”
Isabel Ortiz has warned that the IMF and world financial leaders are talking about “necessary” fiscal consolidation or austerity cuts after the pandemic[217]. “Austerity cutbacks reduce economic activity and worsen living conditions. The pandemic has revealed the weak state of public health systems – generally overburdened, underfunded and understaffed because of earlier austerity policies and privatizations.” In a linked piece Richard Jolly lists eight options that governments can consider, other than austerity.
These issues are too complex to untangle here but it is clear that policy formation and advocacy, in relation to both the COVID-19 and future pandemics, must both factor in and address the evolving structures and dynamics of global political economy.
2.12 Delayed roll out of vaccines and the burden of higher prices
Uncertainty clouds the prospect of safe, affordable and effective vaccines for COVID-19. We don’t know which vaccines (if any) will prove to be effective. Since different countries are looking at different supply arrangements the success of particular candidates will impact on countries’ access to vaccination.
However, it appears likely that most HICs and some UMICs will be able to access effective vaccines in good quantities reasonably soon, at least for their priority populations. The outcomes in China and Russia will depend on the success of their ‘national’ vaccines. The outcomes for countries with production capacity (such as India and Brazil) will depend on the licenses that they have secured. However, most L&MICs are likely to experience a significant delay in accessing vaccines, first for their priority populations, and second for mass vaccination[218].
In terms of cost, it seems that most of the countries with advanced purchase agreements (plus those with ‘national’ vaccines) will be distributing vaccines freely or at highly subsidized retail prices. From the perspective of national treasuries the cost of securing supply is likely to be high, assuming that some of the pre-purchased vaccines turn out to be unsafe or ineffective.
Nkengasong and colleagues from Africa CDC[219] point out that, “To vaccinate 60% of its population (the estimated minimum requirement for herd immunity), Africa will need about 1.5 billion doses of vaccine. … The cost of the vaccine and of building systems and structures required for delivery is estimated at between $7 billion and $10 billion, according to Africa CDC. For comparison, the 2020 US PEPFAR budget was $6.9 billion.”
Vaccine prices for L&MICs are hard to predict. Estimates for Chinese vaccines range from $15 to $75 per shot[220]. Vaccines supplied under the Covax Facility to the ‘funded countries’ for their priority populations will be supplied through Gavi at cost. However, if Covax is underfunded and/or unable to secure adequate supplies, the priority fraction of L&MIC populations who receive vaccines under Covax will be well under the 20%.
Vaccine prices for other L&MICs, and for the funded countries, after the Covax priority supply is exhausted, will be at the discretion of the suppliers. It is likely that they will put in place ‘tiered’ pricing arrangements, stratifying countries according to the companies’ assessment of their ‘ability to pay’. Global supply during this period will be constrained owing to the volume of doses secured by HICs under APAs as well as the imposition of export controls by producer countries. However, there will still be an active spot market beyond the APAs in which the companies will have considerable pricing power. As production ramps up competition between suppliers (including vaccines from China and Russia) prices are likely to fall. In this context countries will face a trade off between early and expensive or later but cheaper.
There is a significant risk that the prices paid by L&MICs for COVID-19 vaccines will inflated by price gouging and that ultimate expenditures on vaccines constitute a significant burden on such countries. Such price gouging will result in further constraints on health care expenditure, social security and economic development.
Perhaps because of the widely shared concerns about equitable access several of the large pharmaceutical firms have announced no profit or low profit pricing for varying periods. AstraZeneca has promised not to profit from its COVID-19 vaccine “during the pandemic” but the company may determine that the pandemic has ended as early as July 2021[221].
Johnson&Johnson has pledged to “allocate up to 500 million doses” of its COVID-19 vaccine to lower-income countries – should its candidate now under development pass Phase 3 trials with results showing it is safe and effective. It is not clear whether the company will donate the vaccines outright or offer them at a reduced price[222].
In September the Gates Foundation announced[223] that a group of 16 global pharmaceutical companies had committed to ensuring global access to diagnostics, therapeutics, and vaccines, including by enabling affordability for lower income countries through approaches such as “donations, not-for-profit supply, or equity-based tiered pricing based on countries’ needs and capabilities”.
Nevertheless, even if there was no price gouging both governments and many families will be facing significant cost barriers to access. For those countries without publicly funded immunization programs, many families will be obliged to pay out of pocket for vaccination. Uncontrolled market prices will add to the burden of these families.
These scenarios of delay and of cost set the context for the possible policy responses outlined in Section 4 below. However, before exploring policy options it is necessary to recall the long history of global debate around access to medicines, before COVID-19.
3. Background: the access to medicines struggle before COVID-19
Current policy making regarding the COVID-19 vaccine arises within a pre-existing global wrangle regarding access to medicines (A2M). The purpose of this section is to provide some background regarding the issues at stake in this wrangle, insofar as they affect the prospects of COVID-19 vaccine access.
This section is designed in particular for those readers who are not closely familiar with this debate or with the structures and dynamics of contemporary pharma.
3.1 The rise of IP protection of pharmaceuticals and debates over pharma innovation, pricing and access
The current regime for the protection of pharma IP should not be seen as ‘natural’; in fact, it is a very recent development. Over the last 25 years there has been a tectonic shift in international norms regarding pharma IP; a heightening and widening of such protection.
TRIPS Agreement
This shift has been implemented largely through the development, ‘negotiation’ and ‘agreement’ regarding the World Trade Organisation’s (WTO) Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS)[224].
The TRIPS Agreement was the outcome of a ten year struggle led by pharma (in particular by Pfizer) to strengthen the protection of intellectual property in pharmaceuticals. Two critical provisions were the requirement to grant patents for both the process of synthesizing the product and for product itself, and to adopt a standard 20 period of protection.
TRIPS sets out the principles to be compiled with in national IP law but governments have some discretion in terms of how these principles shall be articulated in national law. This discretion is critical in terms of whether countries are able to fully deploy the flexibilities provided for in the TRIPS Agreement.
Flexibilities, which apply before a patent is granted, include: setting the criteria for patentability, specifying exclusions from patentability, provision for pre-grant opposition, defining full disclosure requirements, and extending the least developed countries (LDC) transition period. Flexibilities which apply after a patent is granted include: providing for post-grant opposition, enabling the research and early working exception, compulsory licensing (CL), government use, CL for export, use of competition law for access, parallel importation, and data protection instead of data exclusivity. However, if national law does not provide for the enjoyment of such flexibilities then they are not available.
The new disciplines regarding IP protection have been strengthened through ‘TRIPS Plus’ provisions in various bilateral and plurilateral ‘free’ trade agreements. Such agreements commonly bestow extended privileges on big pharma (new uses, evergreening, patent linkage, etc) and often require text which foregoes the use of CL, parallel importation or other flexibilities.
Beyond the formal provisions of TRIPS and other agreements, the interests of big pharma have been further protected through bilateral bullying, most notoriously through the Special 301 provisions of the US Trade Act[225],[226] which empower the US government to impose trade sanctions on countries whose national policies are seen as unfriendly to pharma. Making use of TRIPS flexibilities clearly identifies countries as pharma unfriendly. The Pharmaceutical Research and Manufacturers Association of America (PhRMA) submits annually a ‘watch list’ of pharma unfriendly countries to the US Trade Representative (USTR) which is faithfully reflected in the official Special 301 report.
Big pharma was instrumental in the development and conclusion of the TRIPS agreement (Drahos[227]), in driving TRIPS plus provisions in plurilateral agreements, and in the implementation of trade sanctions under Special 301 provisions.
There has been ongoing and widespread resistance to extreme IP rights protection because of the high prices enabled by the monopoly that exclusive IP endows and the consequent barriers to access; barriers which affect both families and governments. Drug costs comprise a high proportion of total health costs in low and middle income countries (L&MICs); the opportunity costs of paying high prices for medicines include not employing enough health workers.
The access movement started in South Africa in 1997 in the context of the AIDS/HIV crisis (Heywood 2009)[228]. At a time when Medicins Sans Frontieres (MSF) was able to procure AIDS medicines for $500 per treatment year, the pharma companies were setting prices at around $10,000 per treatment year, a price which was out of reach of most families and which would bankrupt the government if they sought to procure at that price. When the South African government sought to make use of parallel importation to achieve lower prices, a group of 39 international pharmaceutical companies, supported by the Clinton administration, tried to block this in the South African courts. There was a massive outcry, led by the Treatment Action Campaign (TAC) in South Africa and supported by international organisations including MSF and (what is now) Knowledge Ecology International (KEI).
In May 2001, under global opprobrium, the drug companies withdrew and agreed to pay costs. In December of that year the ministerial council for the TRIPS Agreement met in Doha and, in the Doha Declaration on TRIPS and Public Health[229] affirmed the legitimacy of TRIPS flexibilities; affirmed that trade policy should not over-ride public health considerations; and initiated a revision of the Agreement to provide for compulsory licensing for export (what became Article 31bis).
The conflict shifts to WHO: TRIPS flexibilities
The conflict over price-gouging and access brought the implications of the TRIPS Agreement to the attention of L&MICs everywhere and in 1999 the World Health Assembly (WHA) adopted resolution WHA52.19[230] which requested that the Director General assist members in developing policies and regulations that assess the pharmaceutical and health policy implications of trade agreements and assist countries to ‘maximize the positive and mitigate the negative impact of those agreements’.
In January 2005, the WHO Secretariat submitted a report on trade and health[231] to the WHO Executive Board (EB). While it was praised by several developing countries, the United States delegation criticised the report, and accused the Secretariat of being ‘against industry, free trade, and intellectual property’[232].
In May of that year (at the WHA, May 2005), Thailand introduced a resolution ‘International trade and health’, on behalf of itself and thirteen countries, which urged member states to work towards policy coherence in trade and health, and to reduce the risks to health systems and health outcomes from trade agreements. The draft requested the Director-General to provide support to member states in relation to these goals. The draft was strongly opposed by the US and its allies and the debate was deferred. At the subsequent WHA (May 2006) a revised resolution (WHA59.26)[233] was adopted, despite the opposition of the US.
WHA59.2645 urged member states to ensure that, in adopting policies, laws, and regulations where trade and health considerations overlapped, they enable the full deployment of such flexibilities as were provided in trade agreements to address public health needs. Further, the resolution called upon the Director General to support member states in framing coherent policies to address the relationship between trade and health.
The significance of WHA59.26 stems in part from the recognition of the need for L&MICs to ensure that their intellectual property legislation provided for the full deployment of the flexibilities in TRIPS as a pre-requisite for affordable access to medicines. However, WHO has been effectively prevented from implementing the resolution through the control over WHO’s program of work exercised by the US and Europe through the long-standing freeze on assessed contributions and tight ear-marking of donor support[234].
Further conflict in WHA: the funding of innovation for public health
A related conflict within the WHA, from 2003 to the present, centres on the funding of innovation for public health. On one hand pharma and its supporters claim that high levels of IP protection are necessary to generate the funds needed to support continuing innovation. On the other hand, this model of innovation funding systematically neglects diseases which disproportionately affect people in developing countries. In fact, it also neglects other pharmaceutical products which do not promise high profits, most notably, antibiotics.
Resolution WHA56.27[235], adopted in May 2003, asked the DG “to establish the terms of reference for an appropriate time-limited body to collect data and proposals from the different actors involved and produce an analysis of intellectual property rights, innovation, and public health, including the question of appropriate funding and incentive mechanisms for the creation of new medicines and other products against diseases that disproportionately affect developing countries”.
The WHO Commission on Intellectual Property Rights, Innovation and Public Health was appointed in 2003 and reported in 2006[236]. The Commission reviewed a range of mechanisms designed to spur product development for conditions disproportionately affecting developing countries. These included delinking (replacing monopoly pricing as a source of funding for innovation with a reward scheme), a binding medical R&D treaty to raise public funds for pharmaceutical innovation, and an open source approach based on a general public license which allows others to use or develop the original technology freely.
The recommendations of the Commission were considered by a series of consultative structures including, in 2012, the consultative expert working group on research and development (CEWG). The CEWG recommended[237] a binding treaty for the purposes of funding R&D for conditions disproportionately affecting developing countries, and a delinking of the patent mechanism from the funding of R&D for such diseases. R&D would be funded publicly on a contract or prize basis and the resultant technologies would be made available on an open source basis. This would remove the argument for monopoly pricing to recoup R&D costs.
The proposed treaty was supported by many developing countries but opposed by pharmaceutical corporations and their host governments. The opposition, led by the US and Europe took the form of delaying tactics, including repeated re-examination of old proposals that had been discarded by the CEWG, and the promotion of other mechanisms to boost investment in drugs.
The proposals for delinking, a binding R&D treaty and contract/reward funding have not been adopted by the World Health Assembly. However, the mechanisms which have been deployed in the search for treatments and vaccines for COVID-19 are comparable in many respects.
The prize fund idea is a public policy tool directed to shaping R&D priorities in the private sector; to provide R&D incentives where commercial incentives are weak. It is a supplementary strategy in the sense that it comes into play in the case of ‘market failure’. An alternative approach could be a publicly owned, publicly funded pharmaceutical development industry, subject to public policy guidelines regarding priorities and offering open licensing to ensure universal access to its products. Governments and consumers are paying now to support private sector R&D through high margins on patent protected drugs; they are also paying to support aggressive marketing and generous dividends and bonuses.
The UN High Level Panel on A2M
In 2016, the debate shifted from WHO to the United Nations with the appointment of the High-Level Panel on Access to Medicines with a brief “to review and assess proposals and recommend solutions for remedying the policy incoherence between the justifiable rights of inventors, international human rights law, trade rules and public health in the context of health technologies”.
The report of the High-Level Panel[238]:
- reaffirmed the importance of countries ensuring that their legislation enabled the full deployment of TRIPS flexibilities and prevented practices such as ever-greening and awarding low quality patents;
- called for a review of the provisions for compulsory licensing for export so that they might be easier to use;
- called for curbs on the use of threats and other pressures designed to prevent countries from using TRIPS flexibilities;
- urged that knowledge and technologies developed through publicly funded research should be freely and widely available and urged universities and research institutions to prioritise public health objectives over the financial returns from patenting and licensing;
- called for the negotiation of a binding R&D Convention that delinks the costs of research and development from end prices, to promote access to good health for all;
- called for transparency with respect to R&D costs, public subsidies (including tax concessions), clinical trials initiated, completed and their results, and patent information.
The reception of the HLP’s report in WHO’s governing bodies was mixed[239] with opposition from the US, the EU, Japan and Switzerland but support from many developing countries.
3.2 Public subsidy programs for consumer access reinforces the logic of delinking
Most HICs and many MICs operate publicly funded pharmaceutical subsidy programs to reduce or remove price barriers to consumer access to prescribed pharmaceuticals. Large scale subsidy programs facilitate bulk procurement and monopsonic leverage over pricing.
However, notwithstanding bulk discounts, public subsidy programs are paying for the IP in those pharmaceuticals even though much of the IP in those products was already paid for through publicly funded research. They are also paying for large marketing expenditures, generous dividends and executive bonuses. They are funding a system which neglects low margin but high need pharma development, and which therefore requires further public subsidy for R&D for such needs.
Meanwhile, the policy model of universal health cover (UHC) has become the leading slogan regarding health system development. One of the core ambitions of UHC is to remove user charges (including charges for pharmaceuticals) as barriers to access. As UHC gains traction and more countries look towards the development of pharmaceutical (consumer) subsidy schemes the inefficiencies and distortions of the current model (innovation funded through high margins based on IP protected monopoly pricing) are of widening concern. In this context the logic of delinking becomes more and more attractive; delinking the price of pharmaceuticals (for both consumers and bulk procurers) from the funding of innovation.
3.3 The ‘financialisation’ of pharma
The failure of pharma to invest in needs-based pharma innovation is inherent in the ‘financialisation’ of pharma[240],[241]; it is an imperative of the pharma business model rather than a commercial choice.
The ‘financialisation’ of pharma refers to the increasing focus, in corporate strategy, on the buying and selling of companies to acquire intellectual property rather than funding in-house innovation to create intellectual property.
With the ‘financialization’ of pharma the site of innovation (and the burden of risk) has moved away from the big ‘research-based’ pharma companies to small, often academically derived, start-ups which drive the innovation and carry the risk (but are then absorbed by the big corporations when they develop promising technologies). The start-ups provide a stepping-stone between publicly funded academic research (where costs are high and outcomes very uncertain) and big pharma where profitable knowledge is commercialised at relatively low risk;
Under this business model the focus of big pharma is on mergers and acquisitions directed to acquiring emerging technologies, expanding into new markets or forestalling competition (from generic or other proprietary companies). (The acquisition by Gilead of Pharmasset, the developer of sofosbuvir for hepatitis C, in 2012 is a high profile example[242].) The role of large ‘research-based’ pharma corporations under this model is to undertake the not-so-risky late stage research including clinical trials and ‘market development’.
In this business model, market value and debt play a critical role in generating funds for such mergers and acquisitions. The need to grow market value (to facilitate borrowing and provide leverage in mergers and acquisitions) exposes pharma to increasing demand for generous dividends and buybacks to satisfy shareholders and to keep the share price high. High debt levels lock in the requirement to keep the share price rising and to pay generous dividends (or buy backs).
The critical role that share price plays in this model leads to a focus on share price in determining executive bonuses. During the current pandemic, Moderna executives have realised huge capital gains through selling stock following optimistic reports on their COVID-19 vaccine candidate[243],[244],[245].
The importance of share price contributes to deliberate opacity in terms of clinical trial data; and animates highly optimistic media announcements (commonly well in advance of peer-reviewed published results). The refusal of pharma to participate in WHO’s solidarity vaccine trial, with its capacity to compare vaccines) would clearly constrain corporate share market strategies.
Central to the debates over IP protection is the role of profit from IP-protected monopoly pricing in generating the incentive and the capital for investment in R&D and production of new drugs[246].
Clearly some of the profit generated by IP protected pricing monopolies does feed into R&D for new drugs. However, there are significant inefficiencies and distortions associated with this model:
- the pricing discretion which accompanies monopoly privilege leads to ethically untenable inequities in access to medicines because of price barriers;
- monopoly pricing (defended on the grounds of innovation) actually enables very high profits relative to other industries; much of the profit gained actually feeds higher dividends and bonuses;
- monopoly pricing generates the funds needed for huge expenditure on marketing, often driving inappropriate and excessive use of pharmaceuticals;
- with the movement toward UHC, the public sector is being asked to pay two to three times in support of pharmaceutical R&D; first through publicly funded research; second, through various tax incentives; and third, through pharmaceutical subsidy schemes (where the negotiated price incorporates a component which notionally reflects the cost of innovation);
- IP-linked innovation is profit-focused rather than needs-based; is directed to the blockbusters (eg antihypertensives, antidiabetics and the antihyperlipidemics) and the ‘niche-busters’ (eg personalized biopharmaceuticals and orphan drugs) and fails to invest in low profit drug development needs (antibiotics, SARS and Ebola vaccines[247],and other diseases which disproportionately affect developing countries).
A large fraction of global pharmaceutical R&D takes place in the US and the US government has been the major flag bearer for extreme IP protection globally. This may reflect the national revenues associated with the ‘export’ of IP (high levels of repatriated profits); it may also reflect revolving doors and election funding. However, US prosecution of TRIPS-plus provisions in trade agreements, its bullying through Special 301 trade sanctions, and its opposition to WHO advising countries about legislation for and use of TRIPS flexibilities also reflect the US gripe that countries who control pharma prices (through price controls, bulk purchasing, or TRIPS flexibilities) are free-loading on US innovation[248],[249],[250]. The fact that the US has adopted laws prohibiting the government from controlling pharmaceutical prices paid through Medicare and Medicaid adds a certain passion to this claim.
4. Policy platform for achieving equitable access to COVID-19 vaccines
The drivers of inequity, in terms of access to COVID-19 vaccines, may be identified as operating between countries and within countries.
Internationally, the promise of equitable roll out of effective COVID-19 vaccines has been diminished by the prospective hoarding associated with massive advanced purchase agreements, largely by high income countries. The Covax facility, which had promised more equitable access has been undercut in terms of both funding and vaccine supplies by these APAs. However, Covax does not include UMICs and only provides for the priority fraction of the population (likely to be well below the notional 20%).
At the national level equitable access will depend first, on the institutional systems for vaccine supply and the delivery of vaccination (including the role of out of pocket payment) and second, the explicit allocation priorities of government.
In preceding sections, we have argued that the threats to equitable access are significant. In this section, we set out a policy platform designed to address those threats.
Some of the initiatives we propose could (and should) be implemented now, during the COVID-19 pandemic, while others may be more feasible in the longer term and may be more applicable to new vaccines in comparable future circumstances.
4.1 Immediate initiatives (for an impact during the current pandemic)
Scaling up manufacturing capacity in L&MICs, backed up by organized technology transfer arrangements including global and regional cooperation for manufacturing scale up (including South South cooperation)
In the immediate context we see the scale up of manufacturing capacity in developing countries as the most critical strategy for promoting equitable access to COVID-19 vaccines.
The simplest way to make this happen would be through widespread (voluntary) sublicensing of the local production of approved vaccines, accompanied by broadly encompassing technology transfer and backed up more generally by organized programs of technical cooperation, including South South cooperation. It would be necessary to develop agreed standards for such sublicensing agreements including full transparency and provision for monitoring process and outcomes.
In the context of 198 candidate vaccines (as of October 19) and 44 candidate vaccines in the clinical evaluation stage (as of October 19), vaccine developers are looking to ensure that manufacturing capacity is not a limit in terms of their market share. Agreements between vaccine companies and contract manufacturers, including in developing countries, are being negotiated. Leveraging national ‘loyalty’ to local manufacturers may also assist in gaining market advantage.
Countries which have an effective vaccination system, a large population, and a steady number of COVID-19 cases, will be particularly attractive to the vaccine developers. Securing a wide range of clinical trial sites is also useful having regard to possible genetic differences of the population and the genetic variants of the virus.
The Brazilian Fundação Oswaldo Cruz (Fiocruz), under the Ministry of Health, has a deal with AstraZeneca. Instituto Butantan, under the Sao Paulo State Secretariat of Health, has a deal with Chinese firm Sinovac. In Indonesia, one of the public pharmaceutical companies owned by the Indonesian government, Biofarma, made a deal with Chinese firm Sinovac. The Cuban Finlay Institute has a deal with the Russian developer Gamaleya. All of these deals involve clinical trials as well as manufacturing in the target countries.
How effective such deals are likely to be in terms of technology transfer depends on the details of the agreements and the pre-existing state of technological development. The detail of many of the deals between vaccine developers and local production houses have not been disclosed.
If local production is to play a role in supporting equitable access, a more organized approach to promoting local production and supporting the associated technology transfer would be needed. Such an approach would need to address landscaping, facilitation and partnership development, and organized support for technology transfer[251].
Landscaping existing vaccine manufacturing capacity (both public and private entities) in developing countries is a critical first step. The focus of most published vaccine landscapes (WHO[252], CEPI[253], Airfinity[254],[255],[256]) has been on the sponsors, the technology being deployed and the progress of the vaccine towards marketing approval. CEPI undertook a survey to figure out the manufacturing capacities across the globe but the focus was on the number of doses the respondents could produce[257].
These surveys do not report on whether the candidate vaccines are being developed by the public or the private sector entities or how much public infrastructure or funding is being invested in the respective technology. There are many universities, in most cases public entities, listed as developers, but little or no data about the funding of their research.
There is a clear need for WHO, with support from its regional offices and from member states (and the UN’s Technology Access Partnership), to undertake a survey of manufacturing capacity in developing countries, directed to estimating potential capacity to contribute to COVID-19 vaccine production and technical support required.
Likewise, if there were to be a stronger focus on technology transfer, greater transparency regarding the conditions provided for under the various manufacturing contracts arranged by vaccine developers such as AstraZeneca would be needed.
A voluntary sublicensing strategy, directed at boosting local production for L&MICs would also need organized partnership development, linking vaccine sponsors who are willing to include technology transfer as part of the partnership with local manufacturing enterprises.
We see an urgent need for organized programs of technical cooperation (global and regional) in support of manufacturing scale-up.
In the Asia Pacific region, the following countries have the capacities for R&D and vaccine manufacture: China, Australia, Japan, South Korea, Thailand, Vietnam, Malaysia and Indonesia[258]. Several of these countries have COVID-19 vaccines under development. All of these countries also have scalable manufacturing capacity.
From the perspective of the equitable access to the safe, effective, and affordable vaccine in time, we see the need for two tracks: first, the immediate development of manufacturing and supply capacity, and second, the longer term development of pharmaceutical innovation. Countries investing public resources into the development of manufacturing capacities now could in due course build on such infrastructure to support the scaling up of R&D capacity.
An immediate waiver of the relevant provisions of the TRIPS Agrement (discussed in Section 2.10 above) or the widespread use of compulsory licenses and the exploratory deployment of Article 73 of the TRIPS Agreement to facilitate access to key technologies; and a moratorium on the deployment of ISDS in relation to the COVID-19 response
There are limitations to voluntary licensing, which are exemplified by the case of Gilead’s remdesivir[259]. Gilead has negotiated voluntary licenses (VL) with local manufacturers for production and supply of remdesivir to designated L&MIC markets. These VLs ensure that those markets covered by such licenses have adequate supplies of low-priced generic remdesivir; they also serve to reduce the pressure for CLs. However, they are also serve to restrict access to the generic version and force UMICs to purchase the originator at market rates.
Building local manufacturing capacity by encouraging voluntary sublicensing during the COVID-19 pandemic may not work, particularly if originators are unwilling to support meaningful technology transfer. In such circumstances close consideration must be given to the use of compulsory licensing.
Compulsory licensing facilitates the local manufacturing of medicines, increases access through the production of low-priced generics, and also depresses the price of the originator through competition. If widely adopted, it can disseminate the production and contribute to equitable affordable distribution, as was the experience with HIV/AIDS medicines.
Abbott and Reichman[260] propose that countries deploy compulsory licensing to share IP related to COVID-19 health technologies. They envisage collaborating countries issuing compulsory licenses in accordance with TRIPS and then granting rights under those licenses to an international patent pool. They explain that such licensing would be compliant with both TRIPS article 31 (compulsory licensing) and article 73 (national security exception). They acknowledge that the licensing facilities they propose may run into obstacles caused by the opt-out of TRIPS Article 31bis by a number of high-income countries and they propose various avenues for them to ‘opt back in’.”[261]
However, it is not clear that CL would be a sufficient condition for local vaccine production. Vaccine production requires thousands of manufacturing steps which involve non-patented know-how (trade secrets) as well as high start-up costs[262].
The potential costs and the delays of associated with generic vaccines may be more expensive and take longer than market purchases. Some of those costs and delays could be associated with acquiring non-patented knowhow, not covered by the CL. This issue of access to non-patented knowhow was the reason that technology pooling has been proposed, to pool not only the IP but also other types of knowledge and data also. However, it appears that few or none of the vaccine companies have joined the C-TAP.
The Moderna-Arbutus dispute[263],[264] and the Inovio VGXI dispute[265] illustrate the significance of technology sharing for the development and production of vaccines. However, it remains open for Moderna to ask the US government to issue a CL for the Arbutus-owned technology that is essential for Moderna’s RNA vaccine production.
Historically, CL has often functioned more as a threat rather than as a practical pathway to local production. In most cases, the purpose of the threat was to force the originator to decrease the price or to force them to seek marketing approval in that jurisdiction and supply the medicine in need.
Such threats need to be credible so countries considering this strategy need to think through the practical pathways involved. At the very least this would involve exploring the deployment of Articles 31, 31 bis and 73 to facilitate access to key technologies (including beyond patents) and to explore mandatory pooling as proposed by Abbott and Reichman. This might need to be linked to a campaign to encourage countries, who have committed not to use Art 31bis, to revoke such commitments.
As pointed out by the South African academics in their letter to President Ramaphosa[266] the full deployment of the flexibilities provided for in the TRIPS Agreement requires national IP legislation that fully authorizes such deployment.
See further discussion of TRIPS below under longer term initiatives.
Making Covax work (within the bounds of its limited funding and uncertain access to vaccine supplies)
While we argue strongly for a focus on scaling up local production, either voluntarily or through compulsory licensing (or both), we also urge continuing attention to making Covax work, including encouraging full funding and firm measures to preserve access to vaccine supplies.
However, the restriction of Covax to the priority population fraction is a limitation, particularly as that fraction is reduced from the notional 20% to 15 and perhaps 10% if funding remains insufficient. Once the priority fraction is served each country must resort to purchasing on the open market.
A focus on scaling up of local production will be needed whether or not Covax is fully funded and able to secure sufficient supplies.
Insisting on transparency by vaccine developers, in relation to clinical trial data, costs, prices, patent status, and market approval status
In 2019, the WHA approved WHA72.8 resolution titled “Improving the transparency of markets for medicines, vaccines, and other health products.”[267] The resolution urges member states to promote transparency in relation to prices, clinical trial data, market data, patent status and market approval status. The resolution also urged member states to improve national capacities, including through international cooperation, open and collaborative research for development and production of health products, especially in developing countries and low- and middle-income countries (LMICs), as well as for product selection and cost-effective procurement, quality assurance, and supply chain management.
The draft resolution was proposed by Italy and was driven by the increasing costs of pharmaceuticals in the national health service. The increasing cost pressures are partly a response to the growing importance of ‘orphan’ medicines or medicines for ‘rare’ diseases. These are generally expensive medicines (including biopharmaceuticals, gene therapies, cell therapies) with small markets, increasingly associated with the personalized medicine. The increasing number of expensive drugs for rare conditions being funded through national pharmaceutical subsidy schemes threatens the sustainability of publicly funded healthcare. Increasing transparency in relation to cost of development, cost of production, clinical data and market data would strengthen governments’ capacity to negotiate appropriate prices and reimbursement arrangements.
On July 24 during the COVID-19 pandemic, Italy officially published the long-anticipated Pricing and Reimbursement Decree, which made Italy the first country to implement WHA72.8.
The US strongly opposed resolution WHA72.8 and finally dissociated itself from it. However, transparency has also been an issue in the US as well, where pharma has greater discretion in pricing. There is considerable support in the US Congress for greater transparency. A bill introduced in June[268] would allow Americans to monitor tax dollars used by federal agencies to research COVID-19 medical products by creating a single database. The database would include all financial and non-financial federal support provided to drug makers, along with associated clinical trial data, patent information, and the full terms of agreements made between the federal government and manufacturers.
Equitable and affordable access to effective COVID-19 vaccines would be greatly facilitated by mandating pharma transparency (through statute or funding conditionality).
Moratorium on sovereign debt and avoiding the austerity shut down
In an earlier section we have referred to the burden of debt carried by many developing economies and exacerbated by the COVID-19 crisis[269] and referred to the call by Global Citizen[270] for a suspension of both public and private debt so that poor countries can respond to the pandemic.
Looming beyond the pandemic is the threat of economic austerity, imposed by the IMF and the global banks. The eight policy options that Richard Jolly offers[271] need to be firmly on the policy agenda at the domestic and international levels:
- Domestic policy:
- increase tax revenues, including increasing progressive income and wealth taxation, corporate taxation including taxes to the financial sector that remains largely untaxed;
- increase social security coverage and revenue by bringing workers from the informal economy to the formal sector, thus paying social security contributions;
- claw back illicit financial flows;
- re-allocate public expenditures including replacing high-cost low-social-impact expenditures such as on the military with social expenditure;
- adopt more accommodative macroeconomic frameworks, with some tolerance to inflation and fiscal deficits.
- International measures to support these policies:
- address ballooning sovereign debt through debt forgiveness/relief and debt moratoria with restructuring;
- increase development aid and transfers;
- issue special drawing rights at the international financial institutions, or issue fiat money to developing countries via a multilateral consortium under the United Nations to provide liquidity to prevent a global depression.
These policy options must be discussed openly in national dialogue, with all relevant stakeholders, including unions, employers, governments and civil organization. Austerity can and must be prevented.
Ensuring equitable and strategic distribution of vaccines within countries
The equitable and strategic allocation of vaccines and access to vaccination opportunity will be important in containing spread and alleviating the burden of both illness and lockdown.
Published commentary on vaccine allocation has encompassed both ‘in-country’ and ‘between country’ allocation.
The WHO Allocation Framework was conceived in the context of the Covax discussions in which case the focus was on identifying the priority population fraction (up to 20%) to be assigned priority in receiving vaccine supplies from Covax. This framework was largely designed for the allocation between countries, and only for the priority fraction. However, the underlying principles are broadly relevant to within-country allocation and to allocation beyond the putative 20% priority fraction.
The prospect of equitable ‘between-country’ allocation of vaccine doses has been progressively weakened with the progress of APAs and the underfunding of Covax as well as the prospective hoarding of anticipated vaccine supplies. (Under these circumstances the WHO Framework is largely irrelevant.)
In this section our focus is on ‘within-country allocation’. While the WHO allocation principles[272] provide general guidance, this is fundamentally an issue for governments. WHO highlights health care workers and first responders and then vaccine trial participants. In the second rank WHO would prioritise the old and those with pre-existing co-morbidities.
We also urge close attention to:
- low income families, living in crowded circumstances, with minimal opportunities for social distancing; this group may include homeless people, some migrants and refugees;
- precarious workers, at risk of unemployment and destitution, who may see no alternative to continuing to attend work even when symptomatic;
- frontline workers, who are at higher risk of infection during their work, but are not considered as formal ‘healthcare workers’; this group may include informal care workers and delivery workers.
Clearly other axes of disadvantage cut across these three groups, including race/ethnicity and gender.
These groups do not appear in the 20% priority population fractions discussed by WHO or Gavi but control of the virus within these groups could make a significant contribution to human rights and to containing the pandemic.
However, without pro-active government intervention, existing economic and institutional inequalities may shape vaccination access along very different lines, including where capacity to pay influences access to vaccination or where powerful interest groups are able to jump the queue.
National and subnational governments must also be held accountable for implementing equitable guidelines for accessing vaccination. This calls for close attention by civil society, hopefully supported by WHO national and regional offices. [273]
4.2 Longer term initiatives (starting now for outcomes in the medium to longer term)
Most of the initiatives proposed above for immediate action (scaling up manufacturing, compulsory licensing, transparency) also call for longer term policy formation and institutional development.
However, there are important policy issues arising from the COVID-19 experience which point towards reforms which may take longer to implement and may be more relevant to the next pandemic than to this one.
Establishing and strengthening public sector innovation and manufacturing in developing countries
We argue that establishing and strengthening public sector pharmaceutical innovation and manufacturing should be a policy priority for developing countries, either on a national or regional basis. The need for local manufacturing is self-evident in the current context of prospective vaccine hoarding. Building local (or regional) innovation capacity is necessary to ensure countries have the technical expertise to support local manufacturing under compulsory licensing and to facilitate ongoing technology transfer.
As discussed above many vaccine developers are striking sublicensing deals with vaccine manufacturers in different countries and regions as part of scaling up their manufacturing capability. We presume that distributed manufacturing under voluntary licensing will be associated with technical support from the license holder. Such deals may serve as bridges for technology transfer.
However, voluntary licenses have limitations and such technical support will not be forthcoming for manufacturing under compulsory licenses. Accordingly, countries need to invest now in ensuring that they have the technical capacity to launch such manufacturing.
Local (or regional) research and innovation capacity is critical in terms of mediating and facilitating technology transfer, either through individual training and experience or through organizational development.
The reasons for insisting on public sector capacity in both innovation and production arise from: a long history of price gouging, the long term failure of the private sector to invest in R&D for vaccines; the refusal of private sector originators to participate in the COVID-19 Technology Access Pool, or in WHO’s Solidarity Vaccine Trial; and the ongoing lack of transparency of private sector originators. The successful experiences of public sector production under compulsory licenses, especially in the case of HIV/AIDS medicines in Brazil, Thailand, and Indonesia,[274],[275],[276],[277],[278] and the current involvement by these public producers in COVID-19 vaccine development (see below) demonstrate their capacity. We can also note the successful South South cooperation between the Cuban Finlay Institute under BioCubaFarma and Brazilian BioManguinhos under Fiocruz, as well as between Finlay Institute and Vietnamese Vabiotech.[279]
The idea of public sector innovation and production is not only for the L&MICs. In times past most HICs had public pharmaceutical producers, especially for vaccines. Some of them remain, but others have been privatized. In many HICs, there are ongoing campaigns by CSO groups and politicians to (re)nationalize the pharmaceutical industry including vaccine production. This was the case even before the COVID-19 but such calls have increasingly got relevance and support under the pandemic. Restoring public sector innovation and production capacity in the HICs would also strengthen the capacity for North-South public-public cooperation.
Regional and plurilateral agreements on biopharmaceutical technology transfer and capacity building
There is clearly a need for organized technical assistance programs in relation to pharma and biopharma (for both R&D and manufacturing). These could be based on bilateral, regional or plurilateral agreements, including South-South or South-North cooperation. This kind of technology transfer could involve scholarships and fellowships and various forms of institutional partnering.
There are already centres of excellence in pharmaceutical (and biopharmaceutical) research and development in the Global South.
In Brazil, the public laboratories Fundação Oswaldo Cruz and Instituto Butantan are developing their own vaccines for COVID-19.[280] The Indonesian public laboratory Biofarma is developing its own candidate vaccine as well.
In Thailand, the Government Pharmaceutical Organisation (GPO), under the Thailand Ministry of Health, is supporting a range of COVID-19 vaccine development initiatives, working with Mahidol University, Chulalongkorn University; and the National Center for Genetic Engineering and Biotechnology (BIOTEC)[281]. Chula Vaccine Research Center (Chula VRC) under the Chulalongkorn University itself working on three vaccine initiatives. Chula VRC is working with the University of Pennsylvania on a LNP-mRNA vaccine[282] which is expected to enter the clinical evaluation in September. This would make Thailand one of the first L&MICs to undertake clinical evaluation of a COVID-19 vaccine.[283],[284]
In Vietnam, the Vaccine and Biological Production No.1 Company (Vabiotech), under the Vietnamese Ministry of Health, is developing a recombinant S protein in IC-BEVS vaccine using a protein subunit platform in partnership with the Bristol University. This is the first time a vector-based vaccine is under development in Vietnam.[285],[286] This vaccine is expected to enter the clinical evaluation in October at the earliest. The company is optimizing production procedures for large-scale production of the vaccine and could produce up to 100 million doses a year.[287]
In late August Cuba’s BioCubaFarm launched a phase 1 clinical trial of one of four vaccines which are under development in that country. Cuba also has been contracted to assist in the trialing and production of the Russian Gamaleya vaccine[288],[289].
Enterprises such as these could participate in South South capacity building.
Open licensing as a condition of public funding of research
There has been increasing pressure on universities in many countries to commercialise the products of their research, including through patents or facilitating start-ups. The tensions between solidarity and self-interest is well illustrated in the early conflicts within Oxford University and the Jenner Institute over commercial exclusive licensing versus open licencing[290],[291].
Exclusive licensing makes sense in terms of the financial health of universities but actually contributes to significant barriers to affordable access to medicines and vaccines.
The public funding of research should be conditional on an agreed policy of open licensing[292] of intellectual property developed under public funding. This has been a core demand of Universities Allied for Essential Medicines (UAEM) for many years. UAEM has sought to mobilise students to build pressure on university administrations. There is resistance from the universities in relation to this proposition. Further mobilization and alliance building with university staff, professional staff associations, and university students will be needed.
Conditionality tied to public funding of private sector, through grants, subsidies and various tax and regulatory concessions
CSOs have repeatedly highlighted the role of public funding in yielding private patents on COVID-19 technologies. Public Citizen estimates that taxpayers contributed $70.5 million to government agency work that helped lead to the discovery of remdesivir, an experimental COVID-19 therapy patented and developed by Gilead Sciences202,[293].
The Covax strategy includes no conditions governing technology transfer[294] or the open pooling of intellectual property and knowhow; in fact it serves to undercut the modest C-TAP proposal. Even before COVID-19, several CSOs were advocating for conditionalities tied to public subsidies (national and international) to R&D and production (including through Covax).
Such conditionalities should address issues of transparency (clinical trials, R&D costs, production costs, prices), fair pricing, sufficient production volumes, and open licensing and participation in technology pooling in times of declared public health emergencies of international concern (PHEICs).
Mandatory participation in ‘Solidarity trials’
In future pandemics there must be provision for mandatory participation in inclusive comparative trials such as WHO’s solidarity trials. Participation in such trials should be a condition of public funding and perhaps also linked to WHO prequalification and national/regional marketing approval.
It would worth exploring provisions within the International Health Regulations giving the DG the authority to require participation in comparative clinical trials in the event of pandemics declared to be public health emergencies of international concern.
Using the TRIPS Agreement (and making it easier to use)
The provisions for compulsory licensing (CL) and government use in the TRIPS Agreement are important resources in the campaign for equitable and affordable access. CL may serve simply as a threat to encourage pharma to curb prices or to seek marketing approval. However, this provision is only available if countries’ domestic legislation provides appropriate authority and procedures for the deployment of compulsory licensing as needed[295]. Too many developing countries have been persuaded or forced to adopt IP legislation which does not facilitate the full deployment of the flexibilities which are provided for in TRIPS[296].
Article 73 of TRIPS provides for Security Exceptions. “Nothing in this Agreement shall be construed: …(b) to prevent a Member from taking any action which it considers necessary for the protection of its essential security interests … taken in time of war or other emergency in international relations.” It appears self-evident that a pandemic threatens the essential security interests of countries. See Abbott (2020)[297] discussion of the application of this provision to compulsory licensing.
Article 31 provides for compulsory licensing for domestic manufacturing but not all countries have domestic manufacturing capacity. It was for this reason that, following the 2001 WTO Declaration on TRIPS and Public Health, the TRIPS Agreement was amended (Article 31bis) to provide for compulsory licensing for export, involving a compulsory licence for both the exporter and the importer. Unfortunately, the way this provision was conceived has proved to be extremely difficult to implement[298]. The renegotiation of TRIPS to facilitate compulsory licensing for export is urgently needed although it is not clear when an opportunity to achieve this will arise. A further impediment to the wider use of Article 31bis is the fact that a range of high income countries committed to not using it following its adoption. Garrison (2020)225 argues that revoking these opt outs would greatly increase the scale on which compulsory licensing for export can be used and thus further reduce prices.
It is important to continue to advocate for countries to ensure that their national law provides for the full deployment of the existing flexibilities of TRIPS and for necessary revisions of the Agreement including around the use of Article 31bis. This kind of advocacy is part of building a global constituency to ensure the necessary reforms are achieved.
It would also be worth exploring the possibility of including provisions in the TRIPS Agreement which enable the DG of WHO to require technology pooling in the event of pandemics which are declared to be public health emergencies of international concern.
In the first instance campaigning around the need for a moratorium on TRIPS obligations in the pandemic context (as suggested by the South Centre) would help to build such a constituency.
In a similar vein MSF is campaigning around ‘No patents or profiteering in a pandemic’. “MSF is calling for no patents or profiteering on any tests, treatments, or vaccines used for COVID-19.” “Pharmaceutical and diagnostic companies must commit to not seek nor enforce patents. If they won’t do the right thing, then governments can take action,” urges MSF.[299]
Continuing advocacy around delinking and R&D treaty proposal
The full delinking of pharmaceutical R&D and the negotiation of an R&D treaty do not appear likely in the short term. However, the logic for delinking can only become more obvious as support for implementing UHC grows. Financial protection for consumers is a key principle of UHC and it is widely recognized that single payer funding is the most strategic and efficient way of achieving financial protection. In this context the savings associated with delinking and public funding of R&D will be increasingly evident to national finance officials.
It will be important to keep this conversation alive.
5. Campaigning: Political pathways for implementing this program
It is likely, although not inevitable, that the availability of effective COVID-19 vaccines will privilege people in the rich world (well beyond the priority fraction of their populations) before the priority populations of L&MICs see any vaccine.
The main uncertainties regarding the roll out concern the number of vaccines that are approved, the funding of Covax, and the scale up of manufacturing capacity, particularly in L&MICs.
It is likely, although not inevitable, that the prices of commercially produced vaccines will escalate significantly as soon as the Covax facility is exhausted which could be well before the priority populations of the LICs and LMICs have been vaccinated. This increase in prices will constitute a significant barrier to vaccination for individuals and families in many countries and a significant burden on governments. MICs who are excluded from Covax may face significant price barriers much earlier. It may be that these price barriers prevent many countries from achieving a level of herd immunity sufficient to eliminate transmission.
The main uncertainties regarding price concern the dynamics of the global vaccine market after the early allocations (it could become quite competitive but there may also be manufacturing bottlenecks).
The policy priorities for advocacy need to address the needs of the next pandemic as well as the present COVID-19 disaster. The opportunity for deploying some of the strategies which have been advanced under the equitable access flag, such as reform of the funding of pharmaceutical R&D, may have been missed during the COVID-19 pandemic. However, it remains important to keep these policy objectives in view.
The transnational ‘research-based’ pharmaceutical industry will clearly oppose the platform we have proposed. They will be supported by other industry sectors who are in various ways dependent on IP protection and trade secrets (eg, electronics, film and entertainment).
The finance industry will be opposed, including both the retail and corporate investors in big pharma and the financial institutions who profit from the buying and selling of shares and the borrowing and lending of money for mergers and acquisitions. The finance industry will oppose this platform at the national level through the financial media, political lobbying and through ‘negative market sentiment’ (exchange rates, credit ratings etc). The international financial institutions will likewise oppose such a program through their pronouncements on economic policy and their control over economic stabilization assistance and development assistance.
Governments opposed will include the few countries who are substantial exporters of pharmaceutical IP (US, Germany, Switzerland, Japan) and governments who are ideologically or strategically locked into a strongly pro-IP stance.
The developing countries (governments and peoples) would be major beneficiaries of this package (and many would support it). They could support the package through various policy initiatives at the national level (eg legislating to fully deploy TRIPS flexibilities) and through various intergovernmental bodies including WHO, the UN, the G77 and the non-aligned movement.
Governments of countries with substantial public expenditure on consumer subsidy schemes, including HICs as well as L&MICs, would also gain from this platform, particularly smaller countries with limited production capacities. Whether they could be persuaded to support it would depend upon popular demand for single payer UHC.
The defensive strategies, opposing our platform, will include: the rhetoric of incentivising innovation and the rhetoric of equity as deployed in relation to the Accelerator. On top of rhetorical argument will come threats of frightening off foreign investment, loss of market confidence, threats of trade sanctions under Super 301 and threats (perhaps action) under investor state dispute settlement agreements (ISDS)[300].
The package we have outlined is not ‘all or nothing’. Many of the initiatives we are suggesting could be implemented incrementally without too much difficulty and would lay the groundwork for more far reaching initiatives.
The political processes through which this package might be implemented are not necessarily conflict-mediated, win lose engagements. Ultimately the fate of such a program will depend on popular support and gaining such support will involve communications, debate, community mobilization and incremental institutional reform.
5.2 Voices, forums, drivers, pressure points, resources
WHO and UN are important forums which, while they do not have strong enforcement mechanisms, are places where the debates can be held in the open and where the policy and ethical issues can be exposed. Meetings of the G77, NAM, and the G20 are likewise important fora. The South Centre has a critical role in this debate as an intergovernmental organisation which is already prosecuting the case for equitable access.
The multilateral agencies of the UN system (including WHO and UNCTAD) are already promoting local production and technology transfer. Participants at the UNCTAD-WHO webinar on 23 April 2020[301],[302], noted that:
- In the area of vaccines, local capacity is significant in Asian developing countries, but less so in Africa;
- Local producers are open to strategic partnerships for collaborative technology transfer, know-how and management of related intellectual property (IP);
- There are ongoing efforts in the East African Community (EAC) to address the gap in vaccine manufacturing capacity through public-private partnerships;
- Governments should re-examine the effectiveness of existing incentives; they should consider increased domestic production capacity as an insurance for the next pandemic[303].
The longstanding trilateral program on access to medicines, IP and trade, involving WHO, WTO and WIPO[304],[305] published a report in 2013[306] which included strategies to encourage local production and technology transfer. An updated study was launched in July 2020[307].
The recurring attacks on WHO and the UN are highly significant in terms of weakening and rendering less relevant multilateral fora where developing countries have a voice. The marginalization of WHO in the design and governance of the Access to COVID-19 Tools Accelerator illustrates the drive to replace member state multilateralism with multi-stakeholder public private partnerships in global health governance. This is very much about marginalising developing country voices.
L&MIC governments are key players in the unfolding history of this struggle. They are key players as advocates in the international debate; as legislators in relation to the legislative changes which may be needed domestically; and, in relation to the implementation of single payer UHC and the need to contain pharma prices.
The policy logic for the above package is strong. Pointing to the dysfunctional character of the ‘research-based’ pharmaceutical industry (and the double/ triple payment for pharma IP), is important, particularly in the context of the move towards UHC and public financing of medicines and vaccines. Government treasuries (in low-, middle-, and high-income countries) who are seeking to contain the costs of single payer UHC will appreciate the logic of both transparency and delinking. Likewise, the gains in terms of economic development from building R&D capacity and local production capacity will be attractive to a range of constituencies.
The debate is not only about the material benefits of reform. It will also be important to contribute to the delegitimation of the current model. Privileging executive bonuses, generous dividends and capital gains over prompt, affordable access is ethically repugnant for many, particularly given the flawed logic of ‘incentivising innovation’. The ethical dimension is of particular importance in mobilising those constituencies who are not personally disadvantaged by the prevailing model.
In the same vein it is important to keep a focus on universities. Universities are sensitive to the ethics of being part of a hyper-profitable industry which puts bonuses and dividends ahead of treating and preventing illness. Students have a particular leverage in driving the UAEM logic of open licensing as opposed to selling out to the big international pharmaceutical giants.
In all of these fields, activist civil society organisations and academic experts specialising in issues of access play a critical role in researching and articulating the issues.
Fundamental to all of these strategies is movement building and networking; new information and new alliances driving change. These issues are both domestic and international; the need is for stronger organising and networking: building the global people’s health movement for equitable access.
We are headed towards a seriously inequitable roll out of COVID-19 vaccines and probably a rapid escalation in vaccine prices. These will prolong the death and devastation.
At this stage in the pandemic a rapid upscaling of local production capacity is the most critical objective. However, there will be future pandemics, probably of increasing frequency. Addressing the wider issues canvassed in this paper could contribute to a faster, more equitable and more efficient roll out of vaccines and medicines next time.
We are at a watershed moment. Action now will facilitate affordable and equitable access during the present pandemic and contribute to structural reform for the longer term.
ACT-Accelerator Access to COVID-19 Tools Accelerator
Africa CDC Africa Centres for Disease Control and Prevention
BARDA US Biomedical Advanced Research and Development Authority
BMGF Bill and Melinda Gates Foundation
CEPI Coalition for Epidemic Preparedness Innovations
CEWG Consultative Expert Working Group on Research and Development
CL compulsory licensing
CSO civil society organisations
C-TAP COVID-19 Technology Access Pool
DCVMN Developing Countries Vaccine Manufacturers’ Network
GloPID-R Global Research Collaboration for Infectious Disease Preparedness
Health GAP Global Access Project
HICs high income countries
HLP High-Level Panel on Access to Medicines
IFPMA International Federation of Pharmaceutical Manufacturers
IFRC International Red Cross and Red Crescent Movement
IGBA International Generic and Biosimilar Medicines Association
IHRs International Health Regulations
IP/IPR intellectual property / intellectual property rights
KEI Knowledge Ecology International
L&MIC low and middle income countries
LIC low income countries
LMI lower middle income countries
MSF Médicins Sans Frontières
NIAID US National Institute of Allergy and Infectious Diseases
PEPFAR US President’s Emergency Plan for AIDS Relief
PHEIC public health emergencies of international concern
PPE personal protective equipment
R&D research and development
TNCs transnational corporations
TRIPS Agreement Agreement on Trade-related Aspects of Intellectual Property Rights
TWN Third World Network
UAEM Universities Allied for Essential Medicines
UHC universal health cover
UMIC upper middle income countries
UN TAP UN Technology Access Partnership
UNCTAD UN Conference on Trade and Development
UNDP UN Development Programme
WHA World Health Assembly
WHA World Health Assembly
WHO World Health Organization
WTO World Trade Organisation
III. ENDNOTES
[1]. https://www.worldometers.info/coronavirus/
[2]. https://www.sciencemag.org/news/2020/07/brain-fog-heart-damage-COVID-19-s-lingering-problems-alarm-scientists (July 31)
[3]. https://www.sciencemag.org/news/2020/07/brain-fog-heart-damage-COVID-19-s-lingering-problems-alarm-scientists (July 31)
[4]. https://www.jwatch.org/fw116877/2020/07/27/cardiac-involvement-COVID-19-detailed-heart-failure (July 27)
[5]. https://www.paho.org/en/news/19-5-2020-paho-director-calls-protect-vulnerable-groups-effects-COVID-19-pandemic (May 19)
[6]. http://www.ipsnews.net/2020/07/neglected-sacrificed-older-persons-COVID-1919-pandemic (July 28)
[7]. https://www.theguardian.com/us-news/2020/aug/11/COVID-19-healthcare-workers-nearly-900-have-died (August 11)
[8]. https://www.nytimes.com/2020/06/16/us/coronavirus-inmates-prisons-jails.html (June 16)
[9]. https://doi.org/10.1215/03616878-8641481 (May 28)
[10]. https://www.brookings.edu/blog/up-front/2020/06/16/race-gaps-in-COVID-19-deaths-are-even-bigger-than-they-appear/?utm_campaign=Economic%20Studies&utm_medium=email&utm_content=89649463&utm_source=hs_email (June 16)
[11]. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html (July 5)
[12]. https://www.nejm.org/doi/full/10.1056/NEJMp2023616 (July 22)
[13]. https://www.nytimes.com/2020/07/06/world/middleeast/coronavirus-saudi-domestic-workers-maids-arab.html (July 6)
[14]. https://www.nytimes.com/2020/07/06/world/europe/coronavirus-roma-bulgaria.html (July 6)
[15]. https://www.washingtonpost.com/health/income-emerges-as-a-major-predictor-of-coronavirus-infections-along-with-race/2020/06/22/9276f31e-b4a3-11ea-a510-55bf26485c93_story.html (June 23)
[16]. https://www.washingtonpost.com/health/income-emerges-as-a-major-predictor-of-coronavirus-infections-along-with-race/2020/06/22/9276f31e-b4a3-11ea-a510-55bf26485c93_story.html (August 3)
[17]. https://www.nytimes.com/2020/08/31/nyregion/rapid-coronavirus-test.html (August 31)
[18]. https://www.medscape.com/viewarticle/932550?nlid=136037_5403&src=wnl_dne_200622_mscpedit&uac=257107DX&impID=2429452&faf=1 (June 19)
[19]. https://www.medscape.com/viewarticle/933191?nlid=136194_5403&src=wnl_dne_200702_mscpedit&uac=257107DX&impID=2443869&faf=1 (July 1)
[20]. https://www.nytimes.com/interactive/2020/science/coronavirus-drugs-treatments.html (July 16)
[21]. https://milken-institute-COVID-19-tracker.webflow.io/ (August 4)
[22]. https://www.statnews.com/2020/07/23/nih-to-start-flurry-of-large-studies-of-potential-COVID-19-treatments/ (July 23)
[23]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200528-COVID-19-sitrep-129.pdf?sfvrsn=5b154880_2 (May 28)
[24]. https://unitaid.org/news-blog/act-accelerator-moves-to-expand-access-to-dexamethasone-for-low-and-middle-income-countries-for-COVID-19-treatment/#en (July 3)
[25]. https://www.medscape.com/viewarticle/932954?nlid=136122_5403&src=wnl_dne_200629_mscpedit&uac=257107DX&impID=2439047&faf=1 (June 26)
[26]. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31757-8/fulltext/ (August 22)
[27]. https://www.washingtonpost.com/science/2020/06/29/coronavirus-mutation-science/?arc404=true (June 29)
[28]. https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html (July 24)
[29]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (952, October 19)
[30]. https://milken-institute-COVID-19-tracker.webflow.io/ (August 4)
[31]. https://tech.sina.com.cn/roll/2019-12-31/doc-iihnzhfz9428799.shtml (3,31 Dec 2019)
[32]. http://tech.sina.com.cn/roll/2020-01-09/doc-iihnzahk3089851.shtml (39, 9 Jan)
[33]. https://www.chp.gov.hk/files/pdf/letters_to_doctors_20200111.pdf (44, 11 Jan)
[34]. https://www.who.int/docs/default-source/coronaviruse/wuhan-virus-assay-v1991527e5122341d99287a1b17c111902.pdf?sfvrsn=d381fc88_2 (75, 13 Jan)
[35]. https://www.dcatvci.org/pharma-news/1762-pharma-gates-foundation-form-global-vaccine-partnership-cepi, (1734, 25 Jan 2017)
[36]. https://cepi.net/news_cepi/cepi-to-fund-three-programmes-to-develop-vaccines-against-the-novel-coronavirus-ncov-2019/ (116, 23 Jan)
[37]. https://fortune.com/2020/08/24/oxford-astrazeneca-COVID-19-vaccine-deal-pricing-profit-concerns/ (1298, 24 August)
[38]. https://www.gov.uk/government/news/funding-and-manufacturing-boost-for-uk-vaccine-programme (1344, 17 May)
[39]. https://www.hhs.gov/about/news/2020/07/07/hhs-dod-collaborate-novavax-produce-millions-COVID-19-investigational-vaccine-doses-commercial-scale-manufacturing-demonstration-projects.html (733, 7 July)
[40]. https://www.economist.com/united-states/2020/07/18/donald-trump-is-hoping-for-a-COVID-19-treatment-by-november (862, 18 July)
[41]. https://www.theguardian.com/business/2020/sep/29/world-bank-announces-plan-poor-countries-buy-COVID-19-vaccines (1511, 30 September)
[42]. https://www.medscape.com/viewarticle/933493?nlid=136327_5403&src=wnl_dne_200709_mscpedit&uac=257107DX&impID=2452687&faf=1 (760, 8 July)
[43]. https://www.reuters.com/article/us-health-coronavirus-russia-vaccine/russian-scientists-hail-results-of-COVID-19-vaccine-trial-idUSKCN24G1UM (870, 15 July)
[44]. https://rwer.wordpress.com/2020/10/11/waiting-for-a-vaccine-killing-for-inequality/ (1622, 11 October 2020)
[45]. https://www.telegraph.co.uk/global-health/science-and-disease/patent-pool-potential-COVID-19-products-nonsense-pharma-leaders/ (877, 29/5/20)
[46]. https://www.theguardian.com/world/2020/may/17/us-and-uk-lead-push-against-global-patent-pool-for-COVID-19-drugs (878, 28/5/20)
[47]. https://www.who.int/blueprint/priority-diseases/key-action/Outline_CoreProtocol_vaccine_trial_09042020.pdf?ua=1 (15/6/2020)
[48]. https://www.medscape.com/viewarticle/938460?nlid=137708_5403&src=wnl_dne_201006_mscpedit&uac=257107DX&impID=2604963&faf=1 (1570, 5 October)
[49]. https://www.who.int/blueprint/priority-diseases/key-action/Global_Research_Forum_FINAL_VERSION_for_web_14_feb_2020.pdf?ua=1 (1023, 11 Feb)
[50]. https://genevahealthfiles.wordpress.com/2020/07/03/research-innovation-forum-on-COVID-19-at-who-july-2-2020/ (689, 3 July)
[51]. https://www.glopid-r.org/ (1031)
[52]. https://www.who.int/teams/blueprint/COVID-19 (1030)
[53]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200615-COVID-19-sitrep-147.pdf? (557, 15 June)
[54]. https://doi.org/10.1016/S0140-6736(20)31821-3 (1372, 27 Aug)
[55]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200615-COVID-19-sitrep-147.pdf (557, 15 June 2020)
[56]. https://www.who.int/blueprint/priority-diseases/key-action/Outline_CoreProtocol_vaccine_trial_09042020.pdf?ua=1 (April 9)
[57]. https://doi.org/10.1016/S0140-6736(20)31821-3
[58]. https://www.who.int/news/item/15-10-2020-solidarity-therapeutics-trial-produces-conclusive-evidence-on-the-effectiveness-of-repurposed-drugs-for-COVID-19-in-record-time (1655, 15 October)
[59]. https://www.who.int/ethics/publications/key-criteria-ethical-acceptability-ofCOVID-19-human-challenge/en/ (511, 7 May)
[60]. https://www.washingtonpost.com/world/europe/COVID-19-challenge-trials-uk/2020/10/20/00a31136-026c-11eb-b92e-029676f9ebec_story.html?utm_campaign=wp_post_most&utm_medium=email&utm_source=newsletter&wpisrc=nl_most&carta-url=https%3A%2F%2Fs2.washingtonpost.com%2Fcar-ln-tr%2F2c3d305%2F5f8f0b289d2fda0efb4f68b1%2F596a65ad9bbc0f0e09eb0502%2F17%2F71%2F5b29b30f6e714a6658ad030a27034999 (1693, 21 October)
[61]. https://www.who.int/blueprint/priority-diseases/key-action/WHO_Target_Product_Profiles_for_COVID-19_web.pdf, (469, 12 April)
[62]. https://www.who.int/ictrp/en/ (1028)
[63]. https://haiweb.org/dutch-institutions-failing-to-register-results-of-clinical-trials/ (1253, 20 Aug)
[64]. https://apps.who.int/gb/COVID-19/pdf_files/18_06/Global%20Allocation%20Framework.pdf (1123, 18 June)
[65]. https://www.ccghr.ca/joint-statement-proposed-global-allocation-framework-COVID-19-products/ (1124, 24 June)
[66]. https://www.twn.my/title2/health.info/2020/hi200702.htm (708, 6 July)
[67]. https://www.sciencedaily.com/releases/2020/09/200903145011.htm (1738, 3 September 2020)
[68]. https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/COVID-19/report-33-vaccine/ (1739, 25 September 2020)
[69]. https://www.nap.edu/download/25917 (1553, 2 October 2020)
[70]. https://www.imperial.ac.uk/mrc-global-infectious-disease-analysis/COVID-19/report-33-vaccine/ (1739, 25 September)
[71]. https://news.northeastern.edu/2020/09/14/if-rich-countries-monopolize-COVID-19-vaccines-it-could-cause-twice-as-many-deaths-as-distributing-them-equally/ (1737, 14 September)
[72]. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200425-sitrep-96-COVID-19.pdf?sfvrsn=a33836bb_4 (496, 25 April)
[73]. https://www.who.int/initiatives/act-accelerator (1406)
[74]. https://pubmed.ncbi.nlm.nih.gov/23598479/ (18/4/2013)
[75]. https://www.who.int/news-room/detail/24-04-2020-global-leaders-unite-to-ensure-everyone-everywhere-can-access-new-vaccines-tests-and-treatments-for-COVID-19 (710, 24 April)
[76]. https://www.who.int/news-room/detail/24-04-2020-commitment-and-call-to-action-global-collaboration-to-accelerate-new-COVID-19-health-technologies (755, 24 April)
[77]. https://www.who.int/news-room/detail/26-06-2020-act-accelerator-update (644, 26 June)
[78]. https://www.twn.my/title2/health.info/2020/hi200807.htm (1235, 14 Aug)
[79]. https://www.who.int/publications/i/item/an-economic-investment-case-financing-requirements (1732, 24 September 2020)
[80]. https://www.who.int/news/item/30-09-2020-un-welcomes-nearly-1-billion-in-recent-pledges-to-bolster-access-to-lifesaving-tests-treatments-and-vaccines-to-end-COVID-19 (1725, 30 September)
[81]. https://www.gavi.org/sites/default/files/document/2020/Covax-Pillar-backgrounder_3.pdf (813, 4 May)
[82]. https://www.gavi.org/news/media-room/world-leaders-make-historic-commitments-provide-equal-access-vaccines-all (June 4)
[83]. https://www.keionline.org/33370 (541,19 June)
[84]. https://genevahealthfiles.wordpress.com/2020/06/19/gavi-covax-facility-questions-on-access-pricing-governance/ (586, 19 June)
[85]. https://www.access2healthcare.net/post/jumping-the-queue-who-will-get-the-vaccine-first (609, 23 June)
[86]. https://www.theguardian.com/commentisfree/2020/jun/24/worlds-poorest-people-coronavirus-vaccine-gavi (615, 24 June)
[87]. https://www.theguardian.com/world/2020/oct/09/covax-vaccine-global-effort-gets-chinas-support (1604, 9 October)
[88]. https://www.aljazeera.com/news/2020/10/9/china-joins-covax-un-backed-global-COVID-19-vaccine-facility (1621, 9 Octpber)
[89]. https://www.reuters.com/article/us-health-coronavirus-vaccines-advance/vaccine-group-plans-advance-market-agreement-for-COVID-19-vaccines-idUSKBN23A2SP (208, 3 June)
[90]. https://www.gavi.org/vaccineswork/covax-explained
[91]. https://www.keionline.org/wp-content/uploads/Covax-Facility-Preliminary-technical-design-061120-vF.pdf (816, 11 June)
[92]. https://www.keionline.org/33370 (541, 19 June)
[93]. https://twn.my/title2/intellectual_property/info.service/2020/ip200605.htm (670, 29 June)
[94]. https://www.theguardian.com/commentisfree/2020/jul/23/world-needs-coronavirus-vaccine-big-pharma-monopoly-astrazeneca-patent-pandemic (921, 23 July)
[95]. https://www.astrazeneca.com/media-centre/articles/2020/astrazeneca-takes-next-steps-towards-broad-and-equitable-access-to-oxford-universitys-potential-COVID-19-vaccine.html (827, 4 June)
[96]. https://www.astrazeneca.com/media-centre/articles/2020/astrazeneca-takes-next-steps-towards-broad-and-equitable-access-to-oxford-universitys-potential-COVID-19-vaccine.html (827, 4 June)
[97]. https://pharmadispatch.com/news/the-COVID-19-vaccine-manufacturing-and-supply-deals, (1348, 28 Aug)
[98]. https://www.nature.com/articles/d41586-020-02450-x (1352, 27 Aug)
[99]. https://genevahealthfiles.wordpress.com/2020/08/27/the-covax-exchange-gavis-plans-to-let-countries-trade-in-vaccines/?utm_medium=email&utm_campaign=email_subscription (1321, 27 Aug)
[100]. https://healthpolicy-watch.news/massive-mobilization-of-us-31-3-billion-required-for-COVID-19-diagnostics-drugs-vaccines-accelerator/ (932, 26 June)
[101]. https://www.who.int/docs/default-source/coronaviruse/act-consolidated-investment-case-at-26-june-2020-(vf).pdf (784, 26 June)
[102]. https://www.medscape.com/viewarticle/936490?nlid=137130_5403&src=wnl_dne_200901_mscpedit&uac=257107DX&impID=2539462&faf=1 (1371, 31 Aug)
[103]. https://www.gatesfoundation.org/Media-Center/Press-Releases/2020/09/Commitments-to-Expanded-Global-Access-for-COVID-19-Diagnostics-Therapeutics-and-Vaccines (1726, 30 September 2020)
[104]. https://www.fiercepharma.com/pharma/astrazeneca-puts-a-time-limit-its-COVID-19-no-profit-pledge-report?mkt_tok=eyJpIjoiTkdKa1lqVXhObUUxWldJNSIsInQiOiJNTTFGcmh3bUxVTmlXZCtFeUs3allLSkR3OTFFc1B5cTJEaDN0UUN6NWdnOElyR2owcERKY25aK2w3Z3QwTW9vbzZpemYrNGVUTEtJS0JZb3lsaHcyVCtVR0ZCYkIrWkVIQitlNXdyTlh3a2NvZTBScndoZFwvYnBxd0VOYlhtRjlJZ29oQlpNbE1rUElmSHJ0b0dqRjJ3PT0ifQ%3D%3D&mrkid=38473288 (1592, 8 October)
[105]. https://genevahealthfiles.substack.com/p/a-peek-into-covax-machine-the-curious?token=eyJ1c2VyX2lkIjoxNTUwNzMxOCwicG9zdF9pZCI6MTM1NTc2NjcsIl8iOiJvYlk4dCIsImlhdCI6MTYwMzQwNzg5NiwiZXhwIjoxNjAzNDExNDk2LCJpc3MiOiJwdWItNzkzOTYiLCJzdWIiOiJwb3N0LXJlYWN0aW9uIn0.RAYImQ60jH0DxrVcj4Op0yWkrNt9-XkOeMKE8xvZjPA (1710, 22 October)
[106]. https://healthpolicy-watch.news/massive-mobilization-of-us-31-3-billion-required-for-covid-19-diagnostics-drugs-vaccines-accelerator/ (932, 26 June)
[107]. https://www.keionline.org/33005 (879, 14 May)
[108]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/covid-19-technology-access-pool (569, 29 May)
[109] https://www.who.int/news-room/detail/29-05-2020-international-community-rallies-to-support-open-research-and-science-to-fight-covid-19 (861, 29 May)
[110]. https://www.keionline.org/32649 (880, 31 March)
[111]. https://www.southcentre.int/southviews-no-200-16-june-2020/ (478, 16 June)
[112]. https://www.access2healthcare.net/post/jumping-the-queue-who-will-get-the-vaccine-first (609, 23 June)
[113]. https://www.telegraph.co.uk/global-health/science-and-disease/patent-pool-potential-COVID-19-products-nonsense-pharma-leaders/ (877, 29 May)
[114]. https://www.theguardian.com/world/2020/may/17/us-and-uk-lead-push-against-global-patent-pool-for-COVID-19-drugs (878, 17 May 2020)
[115]. https://theconversation.com/COVID-19-vaccines-open-source-licensing-could-keep-big-pharma-from-making-huge-profits-off-taxpayer-funded-research-145898 (1735, 18 September)
[116]. https://www.keionline.org/33514 (818, 13 July)
[117]. https://www.europarl.europa.eu/doceo/document/TA-9-2020-0205_EN.html (875, 10 July)
[118]. https://techaccesspartnership.net/
[119]. https://techaccesspartnership.net/posts/COVID-1919-un-launches-platform-for-manufacturers-to-share-tech
[120]. https://www.wto.org/english/tratop_e/COVID-1919_e/export_prohibitions_report_e.pdf (1037, 23 April)
[121]. https://www.koreatimes.co.kr/www/nation/2020/02/119_284055.html (February 25)
[122]. https://www.nytimes.com/2020/03/07/business/eu-exports-medical-equipment.html (March 7)
[123]. https://www.ft.com/content/f6bc4950-5efe-11ea-b0ab-339c2307bcd4 (March 6)
[124]. https://www.whitehouse.gov/presidential-actions/memorandum-order-defense-production-act-regarding-3m-company/ (April 2)
[125]. https://www.cheknews.ca/it-would-be-a-mistake-trudeau-3m-push-back-after-trump-orders-corporation-to-stop-sending-medical-supplies-to-canada-659890/ (April 3)
[126]. https://www.cnbc.com/2020/04/03/coronavirus-3m-tells-trump-halting-exports-would-reduce-number-of-masks.html (April 3)
[127]. https://www.foreignaffairs.com/articles/united-states/2020-07-27/vaccine-nationalism-pandemic?utm_medium=promo_email&utm_source=pre_release&utm_campaign=mktg_sub_vaccine_nationalism_bollyky_reguser&utm_content=20200727&utm_term=registrant-prerelease (964, 27 July)
[128]. https://www.astrazeneca.com/media-centre/articles/2020/astrazeneca-takes-next-steps-towards-broad-and-equitable-access-to-oxford-universitys-potential-COVID-19-vaccine.html (827, 4 June)
[129]. https://pharmadispatch.com/news/the-COVID-19-vaccine-manufacturing-and-supply-deals (1348,28 Aug)
[130]. https://www.npr.org/2020/07/08/889112811/indian-company-starts-mass-producing-coronavirus-vaccines-before-trials (July 8)
[131]. https://koreajoongangdaily.joins.com/2020/07/21/business/industry/SK-Bioscience-COVID-1919-vaccine/20200721192800335.html (July 21)
[132]. http://www.businesskorea.co.kr/news/articleView.html?idxno=50465 (August 14)
[133]. https://www.oxfam.org/en/press-releases/small-group-rich-nations-have-bought-more-half-future-supply-leading-COVID-19 (1483, 17 September 2020)
[134]. https://fortune.com/2020/08/24/oxford-astrazeneca-COVID-19-vaccine-deal-pricing-profit-concerns/ (1298, 24 Aug)
[135]. https://www.fiercepharma.com/manufacturing/astrazeneca-unveils-massive-750m-deal-effort-to-produce-billions-COVID-19-shots (825, 4 June)
[136]. https://www.fiercepharma.com/pharma/astrazeneca-scores-1b-from-u-s-signs-up-to-deliver-hundreds-millions-COVID-19-vaccines (826,21 May)
[137]. https://www.hhs.gov/about/news/2020/07/07/hhs-dod-collaborate-novavax-produce-millions-COVID-19-investigational-vaccine-doses-commercial-scale-manufacturing-demonstration-projects.html (733, 7 July)
[138]. https://www.economist.com/united-states/2020/07/18/donald-trump-is-hoping-for-a-COVID-19-treatment-by-november (862, 18 July)
[139]. https://www.nytimes.com/2020/07/22/us/politics/pfizer-coronavirus-vaccine.html?campaign_id=3&emc=edit_MBAU_p_20200722&instance_id=20533&nl=morning-briefing®i_id=131558958§ion=topNews&segment_id=34077&te=1&user_id=35cf3d9941d7412c45e31a8b5a102ecc (916, 22 July)
[140]. https://www.marketwatch.com/story/biontech-pfizer-shares-gain-on-us-funding-for-coronavirus-vaccine-doses-2020-07-22?mod=pharmaceutical_seemore (1099, 22 July)
[141]. https://www.statnews.com/2020/07/31/operation-warp-speed-sanofi-gsk-COVID-1919-vaccine/?utm_source=STAT+Newsletters&utm_campaign=6271c6b2c3-Pharmalot&utm_medium=email&utm_term=0_8cab1d7961-6271c6b2c3-151499861 (1013, 31 July)
[142]. https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html (August 24)
[143]. https://www.bloomberg.com/news/articles/2020-05-13/u-s-to-get-sanofi-COVID-19-vaccine-first-if-it-succeeds-ceo-says (May 13)
[144]. https://www.ft.com/content/60434224-a70d-4a8d-821f-6ac239b4a349 (May 15)
[145]. https://www.reuters.com/article/us-france-nationalday-macron-sanofi/macron-says-france-will-be-among-first-to-get-sanofi-vaccine-idUSKCN24F1FS (July 14)
[146]. https://www.nature.com/articles/d41586-020-02450-x (1352, 27 Aug)
[147]. https://www.fiercepharma.com/manufacturing/astrazeneca-unveils-massive-750m-deal-effort-to-produce-billions-COVID-19-shots, (825, 4 June)
[148]. https://theconversation.com/coronavirus-how-countries-aim-to-get-the-vaccine-first-by-cutting-opaque-supply-deals-143366 (1343, 27 July)
[149]. https://www.gov.uk/government/news/funding-and-manufacturing-boost-for-uk-vaccine-programme, (1344, 17 May)
[150]. https://www.fiercepharma.com/pharma/astrazeneca-scores-1b-from-u-s-signs-up-to-deliver-hundreds-millions-COVID-19-vaccines (826, 21 May)
[151]. https://www.marketwatch.com/story/uk-signs-deals-with-biontech-pfizer-and-valneva-for-COVID-19-vaccines-2020-07-20?mod=pharmaceutical_seemore (1105, 20 July)
[152]. https://www.dw.com/en/coronavirus-vaccine-nationalism-COVID-19-us-germany-gavi/a-54634662 (1350, 20 Aug)
[153]. https://www.bioworld.com/articles/435761-european-commission-cleared-to-negotiate-advance-purchase-agreements-for-COVID-19-vaccines (1341, 12 June)
[154]. https://www.twn.my/title2/health.info/2020/hi200609.htm (641, 26 June)
[155]. https://epha.org/getting-it-right-COVID-1919-vaccines-procurement/ (700, 3 July)
[156]. https://www.twn.my/title2/health.info/2020/hi200609.htm (641, 26 June)
[157]. https://www.access2healthcare.net/post/jumping-the-queue-who-will-get-the-vaccine-first (609, 23 June)
[158]. https://www.astrazeneca.com/media-centre/press-releases/2020/astrazeneca-to-supply-europe-with-up-to-400-million-doses-of-oxford-universitys-vaccine-at-no-profit.html (1336, 13 June)
[159]. https://www.medscape.com/viewarticle/934125?nlid=136505_5403&src=wnl_dne_200721_mscpedit&uac=257107DX&impID=2469372&faf=1 (912, 20 July)
[160]. https://www.nytimes.com/2020/07/22/us/politics/pfizer-coronavirus-vaccine.html?campaign_id=3&emc=edit_MBAU_p_20200722&instance_id=20533&nl=morning-briefing®i_id=131558958§ion=topNews&segment_id=34077&te=1&user_id=35cf3d9941d7412c45e31a8b5a102ecc (916, 22 July)
[161]. https://www.marketwatch.com/story/astrazeneca-rallies-while-glaxosmithkline-eases-as-ftse-100-slips-11595248440?mod=pharmaceutical_seemore (1102, 20 July)
[162]. https://www.reuters.com/article/us-health-coronavirus-germany-usa/germany-tries-to-halt-u-s-interest-in-firm-working-on-coronavirus-vaccine-idUSKBN2120IV (781, 15 Mar)
[163]. https://www.nytimes.com/2020/03/15/world/europe/cornonavirus-vaccine-us-germany.html, (777, 2 April)
[164]. https://www.politico.eu/article/trump-coronavirus-vaccine-germany-curevac/ (776, 17 Mar)
[165]. https://doi.org/10.1136/bmj.m1100 (778, 17 Mar)
[166]. https://www.gavi.org/vaccineswork/gavi-ceo-dr-seth-berkley-explains-covax-pillar
[167]. https://www.channelnewsasia.com/news/asia/COVID-19-vaccine-japan-astrazeneca-13000602 (1211, 7 Aug)
[168]. https://www.dw.com/en/coronavirus-vaccine-nationalism-COVID-19-us-germany-gavi/a-54634662 (1350, 20 Aug)
[169]. https://pharmadispatch.com/news/the-COVID-19-vaccine-manufacturing-and-supply-deals, (1348, 28 Aug)
[170]. https://www.canada.ca/en/innovation-science-economic-development/news/2020/08/government-of-canada-announces-major-steps-in-treating-and-preventing-COVID-19-through-vaccines-and-therapies.html
[171]. https://www.reuters.com/article/us-health-coronavirus-novavax-canada/canada-wants-to-be-at-front-of-line-for-coronavirus-vaccines-signs-deals-with-novavax-and-johnson-johnson-idUSKBN25R1SX
[172]. https://www.smh.com.au/politics/federal/advanced-negotiations-australia-aiming-to-lock-in-COVID-19-vaccine-deal-20200816-p55m9g.html, (1236, 16 August 2020)
[173]. https://pharmadispatch.com/news/the-COVID-19-vaccine-manufacturing-and-supply-deals (1348, 28 August 2020)
[174]. https://portal.fiocruz.br/en/news/COVID-19-fiocruz-will-sign-agreement-produce-vaccines-university-oxford (June 30)
[175]. https://pharmadispatch.com/news/the-COVID-19-vaccine-manufacturing-and-supply-deals (1348, 28 Aug)
[176]. https://www.indiachinainstitute.org/2020/07/09/the-use-and-abuse-of-global-public-good/?fbclid=IwAR2GIJjcZoxE1zDnbbR3x9rAEi4AzjTNfyTQV3fUW29_eVLnFTRtW4brsrc (749, 9 July)
[177]. https://apps.who.int/gb/ebwha/pdf_files/WHA73/A73_R1-en.pdf (WHA, 17 May)
[178]. https://www.oxfam.org/en/press-releases/world-leaders-unite-call-peoples-vaccine-against-COVID-19 (14 May 2020)
[179]. https://www.theguardian.com/commentisfree/2020/oct/15/peoples-vaccine-coronavirus-COVID-19-wto (15 Oct)
[180]. https://msfaccess.org/COVID-19-vaccine-6-recommendations-equitable-access (22 June)
[181]. https://twn.my/title2/health.info/2020/hi200611.htm (662, 29 June)
[182]. https://twn.my/title2/health.info/2020/hi200611.htm (662, 29 June)
[183]. https://www.keionline.org/33388 (587, 19 June)
[184]. https://www.keionline.org/wp-content/uploads/W666.pdf (996, 17 July)
[185]. http://msfaccess.org/msf-applauds-south-africa-championing-health-safeguards-meeting-wto-members (1116, 3 Aug)
[186]. https://twn.my/title2/health.info/2020/hi200610.htm (642, 24 June)
[187]. https://www.keionline.org/33388 (587, 19 June)
[188]. https://msfaccess.org/african-union-says-urgent-need-address-patents-and-technology-barriers-access-future-COVID-19 (678, 2 July)
[189]. https://us5.campaign-archive.com/?u=fa9cf38799136b5660f367ba6&id=c865cddeb9 (1193, 8 May)
[190]. https://docs.wto.org/dol2fe/Pages/SS/directdoc.aspx?filename=q:/IP/C/W669.pdf&Open=True (1550. 2 October)
[191]. https://twn.my/announcement/signonletter/CSOLetter_SupportingWaiverFinal.pdf (1746, 15 Oct)
[192]. https://msfaccess.org/india-and-south-africa-proposal-wto-waiver-ip-protections-COVID-19-related-medical-technologies (1610, 9 Oct)
[193]. https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2020/october/20201015_waiver-obligations-trips-agreement-COVID-1919 (1643, 15 Oct)
[194]. https://unitaid.org/news-blog/unitaid-supports-call-for-intellectual-property-waivers-and-action-for-access-to-COVID-19-products/ (1632, 13 Oct)
[195]. https://www.thehindubusinessline.com/economy/who-lends-support-to-ip-waiver-proposal-from-south-africa-india/article32885984.ece (1670, 18 Oct)
[196]. https://www.wto.org/english/tratop_e/COVID-1919_e/trips_report_e.pdf (1663, 15 Oct)
[197]. https://mailchi.mp/southcentre/southnews-wto-trips-council-discusses-major-proposals-for-waiving-certain-trips-obligations-and-extension-of-transition-period-for-ldcs?e=59a8962a20 (1721, 23 Oct)
[198]. https://genevahealthfiles.substack.com/p/a-peek-into-covax-machine-the-curious?token=eyJ1c2VyX2lkIjoxNTUwNzMxOCwicG9zdF9pZCI6MTM1NTc2NjcsIl8iOiJvYlk4dCIsImlhdCI6MTYwMzQwNzg5NiwiZXhwIjoxNjAzNDExNDk2LCJpc3MiOiJwdWItNzkzOTYiLCJzdWIiOiJwb3N0LXJlYWN0aW9uIn0.RAYImQ60jH0DxrVcj4Op0yWkrNt9-XkOeMKE8xvZjPA (1712, 22 Oct)
[199]. https://www.wto.org/english/news_e/news20_e/trip_20oct20_e.htm (1683, 20 Oct)
[200]. https://www.keionline.org/34275 (1685, 20 Oct)
[201]. https://twn.my/title2/health.info/2020/hi201011.htm (1681, 20 October))
[202]. https://www.gov.uk/government/news/uk-statement-to-the-trips-council-item-15 (1679, 16 Oct)
[203]. https://www.twn.my/title2/health.info/2020/hi200606.htm (544, 19 June)
[204]. https://www.astrazeneca.com/media-centre/articles/2020/astrazeneca-takes-next-steps-towards-broad-and-equitable-access-to-oxford-universitys-potential-COVID-19-vaccine.html (827, 4 June)
[205]. https://twn.my/title2/health.info/2020/hi201012.htm (1682, 20 Oct)
[206]. https://msf.org.au/article/statements-opinion/COVID-19-msf-calls-no-patents-or-profiteering-drugs-tests-and-vaccines (1 April)
[207]. https://openCOVID-19pledge.org/2020/04/07/patent-holders-urged-to-take-open-COVID-19-pledge-for-quicker-end-to-pandemic-2/ (7 April)
[208]. http://infojustice.org/archives/42692 (1629, 12 Oct)
[209]. https://www.wto.org/english/docs_e/legal_e/04-wto_e.htm#articleIX (see Article IX, Clause 3)
[210]. https://investors.modernatx.com/news-releases/news-release-details/statement-moderna-intellectual-property-matters-during-COVID-19 (1589, 8 Oct)
[211]. https://www.keionline.org/34112 (1591, 8 Oct)
[212]. https://healthgap.org/moderna-responds-to-activist-pressure-but-in-the-race-for-our-lives-we-need-more-than-baby-steps/ (1593, 8 Oct)
[213]. https://www.nejm.org/doi/full/10.1056/NEJMe2024894?query=featured_coronavirus (849, 15 July)
[214]. https://thehill.com/opinion/healthcare/506315-congress-must-stop-trump-from-withdrawing-from-the-who (August 7)
[215]. https://cepr.org/sites/default/files/policy_insights/PolicyInsight104.pdf (1641, 1 Juky)
[216]. https://www.globalcitizen.org/en/au/ (1624, 12 Oct)
[217]. http://www.ipsnews.net/2020/10/imf-encouraging-world-financial-leaders-walk-blindly-towards-austerity/?utm_source=English+-+IPS+Weekly&utm_campaign=de93e8702a-EMAIL_CAMPAIGN_2020_10_22_08_48&utm_medium=email&utm_term=0_eab01a56ae-de93e8702a-5664297 (1705, 22 Oct)
[218]. https://www.statnews.com/2020/10/09/7-looming-questions-about-the-rollout-of-a-COVID-19-vaccine/?utm_source=STAT+Newsletters&utm_campaign=cf23a210fc-Pharmalot&utm_medium=email&utm_term=0_8cab1d7961-cf23a210fc-151499861 (1612, 9 Oct)
[219]. https://www.nature.com/articles/d41586-020-02774-8 (1565, 6 Oct)
[220]. https://www.reuters.com/article/us-health-coronavirus-china-vaccine-idUSKBN2710UQ?utm_source=Nature+Briefing&utm_campaign=a01241894e-briefing-dy-20201019&utm_medium=email&utm_term=0_c9dfd39373-a01241894e-45687762 (1694, 16 Oct 2020)
[221]. https://www.ft.com/content/c474f9e1-8807-4e57-9c79-6f4af145b686 (1578, 7 Oct)
[222]. https://healthpolicy-watch.news/77209-2/ (1538, 30 Sept)
[223]. https://www.gatesfoundation.org/Media-Center/Press-Releases/2020/09/Commitments-to-Expanded-Global-Access-for-COVID-19-Diagnostics-Therapeutics-and-Vaccines (1726, 30 September)
[224]. https://www.wto.org/english/docs_e/legal_e/27-trips_03_e.htm
[225]. https://www.southcentre.int/research-paper-115-july-2020/ (1142, July 31)
[226]. https://www.southcentre.int/policy-brief-83-august-2020/ (1260, Aug 1)
[227]. Drahos, P. (2002) http://www.anu.edu.au/fellows/pdrahos/articles/pdfs/2002devcountriesandipstandards.pdf
[228]. http://jhrp.oxfordjournals.org/cgi/content/abstract/1/1/14
[229]. https://www.wto.org/english/thewto_e/minist_e/min01_e/mindecl_trips_e.htm (Nov 20, 2001)
[230]. https://www.who.int/phi/WHA52.19.pdf (May 24, 1999)
[231]. http://apps.who.int/gb/archive/pdf_files/EB116/B116_4-en.pdf (EB116/4, May 2005)
[232]. https://apps.who.int/gb/ebwha/pdf_files/EB116-REC1/B116_2005_REC1-en.pdf#page=55 (Jan 2005)
[233]. http://apps.who.int/gb/ebwha/pdf_files/WHA59-REC1/e/WHA59_2006_REC1-en.pdf#page=53 (May 2006)
[234]. http://www.twn.my/title2/resurgence/2015/298-299/cover01.htm (Legge, 2015)
[235]. http://apps.who.int/gb/archive/pdf_files/WHA56/ea56r27.pdf (May 2003)
[236]. http://www.who.int/intellectualproperty/en/ (May 2006)
[237]. http://apps.who.int/gb/ebwha/pdf_files/WHA65/A65_24-en.pdf (May 2012)
[238]. http://www.unsgaccessmeds.org/final-report (Sept 2016)
[239]. https://apps.who.int/gb/ebwha/pdf_files/EB140-PSR/B140_PSR11-en.pdf#page=9 (debate at EB140, Jan 2017)
[240]. https://www.sciencedirect.com/science/article/abs/pii/S0277953620303154 (1359, June 1 2020)
[241]. https://www.somo.nl/wp-content/uploads/2020/04/Rapport-The-financialisation-of-Big-Pharma-def.pdf (1360, April 1. 2020)
[242]. https://www.bmj.com/content/354/bmj.i3718 (1358, July 27, 2016)
[243]. https://www.cbsnews.com/news/coronavirus-vaccine-biotechnology-stock-market-investment-bubble/ (1086, May 28)
[244]. https://www.smh.com.au/business/companies/big-pharma-executives-are-cashing-in-on-COVID-19-vaccine-share-speculation-20200703-p558mc.html (July 3)
[245]. https://www.statnews.com/2020/10/13/selling-stock-like-clockwork-modernas-top-doctor-gets-1-million-richer-every-week/?utm_source=STAT+Newsletters&utm_campaign=607cba3500-Pharmalot&utm_medium=email&utm_term=0_8cab1d7961-607cba3500-151499861 (1637, 13 October 2020)
[246]. PhRMA. (2013). Intellectual property protections are vital to continuing innovation in the biopharmaceutical industry. http://www.phrma.org/innovation/intellectual-property (Accessed 22 October 2013, since removed).
[247]. https://www.southcentre.int/southviews-no-195-14-may-2020/ (1059, May 14)
[249]. https://www.bbc.com/news/business-47377427 (26 Feb 2019)
[250]. https://freebeacon.com/issues/europe-free-riding-american-drug-innovation-congressmen-warn-trump/ (24 April 2018)
[251]. https://www.mckinsey.com/industries/pharmaceuticals-and-medical-products/our-insights/why-tech-transfer-may-be-critical-to-beating-COVID-19 (1572, 23 July 2020)
[252]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (September 9)
[253]. https://www.nature.com/articles/d41573-020-00151-8?utm_source=Nature+Briefing&utm_campaign=6bcfacc11e-briefing-dy-20200904&utm_medium=email&utm_term=0_c9dfd39373-6bcfacc11e-45687762 (1387, 4 September 2020)
[254]. https://www.nature.com/articles/d41586-020-02450-x (1352, August 24 2020)
[255]. https://www.bloombergquint.com/onweb/frontrunning-COVID-19-vaccines-will-soon-see-their-moment-of-truth (September 3 2020)
[256]. https://www.independent.co.uk/news/health/coronavirus-vaccine-world-health-organization-uk-airfinity-a9703911.html (September 3 2020)
[257]. https://cepi.net/news_cepi/cepi-survey-assesses-potential-COVID-19-vaccine-manufacturing-capacity/ (August 5 2020)
[258]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (September 9)
[259]. https://msfaccess.org/voluntary-licenses-recommendations-governments-safeguard-access-medicines (1536, 2 October 2020)
[260]. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3656725
[261]. https://medicineslawandpolicy.org/2020/07/trips-council-to-discuss-ip-and-the-public-interest-in-the-context-of-COVID-19/
[262]. The Covax Facility Questions & Answer for Prospective Participants (August 24, since taken down); see also April 2004 https://www.who.int/intellectualproperty/events/en/Background_paper.pdf (1429, April 2004)
[263]. https://twn.my/title2/briefing_papers/twn/Moderna%20IP-COVID-19%20Aug%202020%20Hammond.pdf (1083, 3 Aug 2020)
[264]. https://www.nature.com/articles/s41587-020-0674-1 (1422, 4 Sept 2020)
[265]. https://twn.my/title2/briefing_papers/twn/Hammond.pdf (945, 1 June 2020)
[266]. http://infojustice.org/archives/42692 (1629, 12 Oct)
[267]. https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_ACONF2Rev1-en.pdf
[268]. https://www.statnews.com/2020/06/22/COVID-1919-coronavirus-price-gouging-patents/?utm_source=STAT+Newsletters&utm_campaign=5d6bf595d4-Pharmalot&utm_medium=email&utm_term=0_8cab1d7961-5d6bf595d4-151499861 (606, 22 June 2020)
[269]. https://cepr.org/sites/default/files/policy_insights/PolicyInsight104.pdf (1641, 1 Juky)
[270]. https://www.globalcitizen.org/en/au/ (1624, 12 Oct)
[271]. http://www.ipsnews.net/2020/10/imf-encouraging-world-financial-leaders-walk-blindly-towards-austerity/?utm_source=English+-+IPS+Weekly&utm_campaign=de93e8702a-EMAIL_CAMPAIGN_2020_10_22_08_48&utm_medium=email&utm_term=0_eab01a56ae-de93e8702a-5664297 (1705, 22 Oct)
[272]. https://www.who.int/ethics/publications/ethics-COVID-19-resource-allocation.pdf?ua=1 (undated)
[273]. https://www.nationalacademies.org/our-work/a-framework-for-equitable-allocation-of-vaccine-for-the-novel-coronavirus
[274]. https://www.who.int/phi/publications/local_production_lit_review/en/ (2011)
[275]. https://onlinelibrary.wiley.com/doi/abs/10.1111/dewb.12050 (21 April 2014)
[276]. https://pubmed.ncbi.nlm.nih.gov/17620749/ (July 2007)
[277]. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1467-7660.2008.00494.x (6 October 2008)
[278]. https://www.ip-watch.org/2007/11/26/indonesia-mulls-compulsory-licences-on-three-more-hivaids-drugs/ (26 November 2007)
[279]. https://www.who.int/phi/publications/cuban_experience_local_prod_medstech_transfer/en/ (2015)
[280]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (September 9)
[281]. https://www.nationthailand.com/news/30388885 (June 1)
[282]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (September 9)
[283]. https://www.bloomberg.com/news/articles/2020-06-26/thailand-says-it-s-on-track-for-COVID-19-vaccine-human-trials (June 27)
[284]. https://www.bloomberg.com/news/articles/2020-07-12/thailand-to-begin-its-COVID-19-vaccine-human-trials-in-september (July 12)
[285]. https://www.who.int/publications/m/item/draft-landscape-of-COVID-19-candidate-vaccines (September 9)
[286]. https://www.trialsitenews.com/vietnams-state-owned-vabiotech-pursues-a-vaccine-now-in-mice-testing-so-far-so-good/ (May 9)
[287]. https://www.nationthailand.com/news/30392947 (August 14)
[288]. https://www.aa.com.tr/en/americas/cuba-to-begin-clinical-trials-of-COVID-19-vaccine-/1947388, (1432, 19 August 2020)
[289]. https://www.dw.com/en/cuba-joins-the-race-for-vaccine-against-the-coronavirus/a-54615364 (1431, 19 August 2020)
[290]. https://www.wsj.com/articles/oxford-developed-COVID-19-vaccine-then-scholars-clashed-over-money-11603300412?mod=mhp (1713, 21 Oct)
[291]. https://medicineslawandpolicy.org/2020/10/how-the-oxford-COVID-19-vaccine-became-the-astrazeneca-COVID-19-vaccine/ (1557, 5 Oct)
[292]. https://rwer.wordpress.com/2020/10/17/waiting-for-a-vaccine-and-the-collaborative-research-alternative/ (1672, 17 Oct)
[293]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202249/ (1465, 27 May 2020)
[294]. https://www.keionline.org/33370, (541,19 June 2020)
[295]. https://www.southcentre.int/research-paper-107-april-2020/ (1060, 24 April 2020)
[296]. https://www.southcentre.int/research-paper-115-july-2020/#more-14632 (July 2020)
[297]. https://www.southcentre.int/research-paper-116-august-2020/#more-14969 (August 2020)
[298]. https://medicineslawandpolicy.org/2020/04/never-say-never-why-the-high-income-countries-that-opted-out-from-the-art-31bis-wto-trips-system-must-urgently-reconsider-their-decision-in-the-face-of-the-COVID-19-pandemic/ (#993, 8 April 2020)
[299]. https://msfaccess.org/COVID-19-no-patents-or-profiteering-pandemic?fbclid=IwAR1Gpp0mg63DGbktEbd9mJXhq1FUOOBfpBFKhHT3DqUK8Nag7cbyKya1gp4
[300]. http://s2bnetwork.org/wp-content/uploads/2020/06/OpenLetterOnISDSAndCOVID-19_June2020.pdf, (619, 20 June 2020)
[301]. https://www.who.int/phi/implementation/tech_transfer/Interagency-statement-on-promoting-local-production.pdf?ua=1 (24 May 2019)
[302]. https://www.who.int/phi/implementation/tech_transfer/en/
[303]. https://unctad.org/meetings/en/SessionalDocuments/tot_ip_2020-04-23_COVID-19Report_en.pdf (23 April 2020)
[304]. https://www.who.int/phi/implementation/tech_transfer/Interagency-statement-on-promoting-local-production.pdf?ua=1 (24 May 2019)
[305]. https://www.who.int/phi/implementation/tech_transfer/en/
[306]. https://www.wto.org/english/news_e/news13_e/trip_05feb13_e.htm
[307]. https://www.who.int/news-room/detail/29-07-2020-who-wipo-wto-launch-updated-study-on-access-to-medical-technologies-and-innovation
IV. NAUTILUS INVITES YOUR RESPONSE
The Nautilus Asia Peace and Security Network invites your responses to this report. Please send responses to: nautilus@nautilus.org. Responses will be considered for redistribution to the network only if they include the author’s name, affiliation, and explicit consent.



One thought on “EQUITABLE ACCESS TO COVID-19 VACCINES: COOPERATION AROUND RESEARCH AND PRODUCTION CAPACITY IS CRITICAL”